Charting the lives of hospital microorganisms

In one of the largest microbiome studies in history, researchers tracked the colonization and flow of bacteria in a newly opened hospital.

Day and night, most hospitals are teeming with people and activity. But underneath it all, there exists an unseen microbial world in the hospital—a world made up of billions upon billions of microscopic organisms that live and move throughout the building and on the bodies of patients. But just how do bacteria colonize and move around a hospital over time?
A team of researchers led by Jack Gilbert from the University of Chicago has now started to address this question by using next-generation sequencing (NGS) for large-scale microbial sampling in a hospital setting. Gilbert and his colleagues conducted a year-long intensive survey at a newly opened hospital to learn more about the microorganisms and metagenomics of hospital life. They published the results of their project in the journal Science Translational Medicine.
“The Hospital Microbiome Project is the single biggest microbiome analysis of a hospital performed and one of the largest microbiome studies ever,” said Gilbert, who is the director of the Microbiome Center at the University of Chicago and group leader in Microbial Ecology at Argonne National Laboratory, in a press release.
Sampling a Hospital
Gilbert and his staff focused their efforts on the Center for Care and Discovery, a new inpatient hospital for medical and surgical patients located at the University of Chicago. The authors started sampling from the hospital 2 months prior to opening and continued their sampling for a full year.
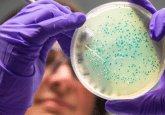
In total, the researchers collected ~10,000 samples from the hospital, detecting microbial DNA in 6523 of these samples. Sampling sites included 10 patient rooms and 2 nurse stations split between 2 floors of the hospital. Within those sites, the researchers assessed microbial diversity on objects such as staff clothing, shoes, and pagers, as well as patients’ hands, noses, and skin. Each room sampled in the study allowed for 24-hour visitation and was cleaned on a daily basis with an ammonium solution and again when patients were discharged with a 1:1000 bleach solution. The researchers then performed large-scale 16S rRNA sequencing on the samples to peer into the hospital microbial community.
“We’ve created a detailed map, highly relevant to clinical practice, of microbial exchange and interaction in a large hospital environment,” Gilbert explained. “This describes the ecology of a building, a thriving microbial ecosystem that regularly interacts with patients in a seemingly benign way—at least most people don’t appear to be negatively affected. It gives us a framework, something we can build on, showing how microorganisms enter and colonize a hospital environment.”
Finding Connections in the Microbiome
Early data showed that the microbial composition of the hospital itself changed once the building was opened to patients. Gilbert noted that prior to the opening, bacterial diversity was low, but shortly after opening, the environment and hospital surfaces became populated with bacteria often associated with the skin.
Interestingly, the research team was able to chart the patterns of bacterial “flow” or movement within the hospital. Upon patient admission, bacteria tended to move from the surfaces within the hospital onto patients. However, this movement changed by Day 2 of a hospital stay, when researchers recorded the opposite effect—movement of microbes from patients onto hospital surfaces, which increased the microbial diversity in the hospital environment.
When viewed using dynamic Bayesian network analysis, the data indicated that hospital staff were more likely the source of bacteria on patient skin than sinks, and bedrails were more likely a bacterial transmission source to patients than the reverse.
Gilbert and his colleagues also looked into how longer patient stays in the hospital affected microbial diversity. In total, the team tested 92 samples; results showed that the abundance of acquired antibiotic resistance genes increased in surface microbes in rooms with long-term patients when compared to other skin samples. Additional sequence analyses showed that some of these bacteria were under continual selective pressure to promote antibiotic resistance. “This requires further study,” Gilbert said, “But if it proves to be true, then these genetic changes could affect the bacteria’s ability to invade tissue or to escape standard treatments.”
While an interesting starting point, the authors noted that the study was based entirely on 16S rRNA sequencing rather than whole-metagenomic sequencing or culturing approaches, limiting the ability to study other important factors in a clinical environment such as bacterial transmission patterns or metabolic functions. Still, the unique nature and depth of this hospital microbiome study suggests paths towards enhancing beneficial microbial interactions in hospital environments in the future.