Novel multi-target cancer therapeutics show promise at clinical and basic research stages
A new mRNA cancer therapy shows promise in mice, while a viral cancer therapy takes great strides forward in human trials, both targeting multiple aspects of cancer.
In a recent study, researchers at Oregon State University (OSU) and Oregon Health & Science University (OHSU; both OR, USA) have developed a novel mRNA therapy that targets ovarian cancer while simultaneously treating cachexia, a muscle wasting condition that frequently co-presents with cancer. This could prove significant in protecting patients from the numerous ways cancer affects the body.
Cachexia causes the loss of muscle and fat even when patients are eating, placing patients in a weakened state that can make them less likely to respond to, and deal with the taxing toxic effects of treatment. The condition itself is responsible for the death of 30% of the patients it impacts [1].
Meanwhile, the lack of an available screening test for ovarian cancer, coupled with the vague symptoms that accompany the early stages of the disease, means that ovarian cancer is often undetected until the later stages of the condition. At these later stages, the only available treatments are surgical resection of the tumor followed by aggressive chemotherapy. Patients receiving this treatment often see a recurrence of their cancer. The 5-year survival rate for late-stage ovarian cancer, once it has spread from the ovaries, is less than 30% [1].
In order to address this two-pronged attack that can be enacted by ovarian cancer, Oleh Taratula (OSU) and Daniel Marks (OHSU) led their respective groups to develop a novel therapeutic that can treat both cachexia and the cancer itself. They designed lipid nanoparticles that encapsulate mRNA coding for the protein follistatin. Follistatin decreases the levels of the protein activin A, which is associated with aggressive ovarian cancer and cachexia [2].
 How can we treat cancer-related cachexia?
How can we treat cancer-related cachexia?
A recent study from Indiana University School of Medicine finds that the excerisise hormone irisin may be responsible for muscle weakening in cancer-related cachexia, but only in males.
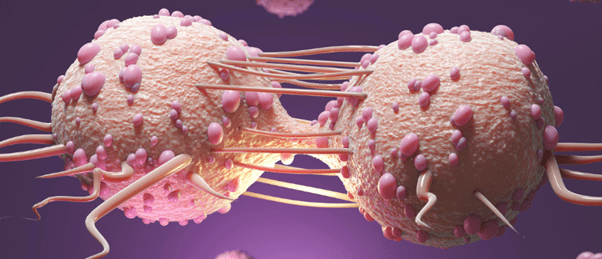
To test the therapeutic, the research team injected it into the peritoneal cavity of ovarian cancer-bearing mice and observed the impact on overall survival and the phenotype of cancer cells in the mice. Commenting on the results Taratula revealed that, “it prevents the build up of ascites – abdominal fluid containing cancer cells. It also delays disease progression and induces the formation of small, solid tumors that don’t adhere to organs and thus can be more easily removed. And it combats cachexia by helping to preserve muscle mass.”
The team also found that it performed well in collaboration with the chemotherapeutic cisplatin extending the lives of mice who received both treatments and reducing muscle atrophy. If this novel drug proves successful in human trials, the inhibition of cachexia could dramatically improve patients’ resilience during chemotherapy while simultaneously inhibiting tumor progression: a development that could prove transformative for the treatment of ovarian cancers [2].
Viral therapy offers a glimpse of the future
While this is currently at the early stages of development, another recent two-pronged approach to target cancer could offer the Oregon team some hope. The treatment, a modified herpes virus named RP2, has seen significant success in a Phase 1 clinical trial, successfully treating nine patients and completely curing another, who has now been cancer free for 15 months.
The clinical trial team, composed of members of The Institute for Cancer Research (ICR) and The Royal Marsden NHS Foundation (both London, UK) tested the safety and dosage of the modified herpes virus against a range of different cancer types. In total 39 study participants were selected, each of whom had exhausted all treatment options, including checkpoint inhibiter therapy. 30 participants were given RP2 in conjunction with immunotherapy and nine were given RP2 alone [3].
The RP2 virus acts by infecting cancer cells and replicating within them until the cells burst, solely targeting these pathogenic cells as a result of the knockout of the genes encoding ICP34.5 and ICP47, two proteins that play vital roles in viral replication and anti-immune responses. It also blocks the protein CTLA-4, which is an immune checkpoint protein that downregulates the immune response, through the production of an anti-CTLA-4 antibody analog [4].
 Nanocarriers deliver 2-in-1 cancer treatment
Nanocarriers deliver 2-in-1 cancer treatment
Researchers develop an innovative nanocarrier to simultaneously deliver a chemotherapeutic and a drug to support the immune system.
In the nine patients who received RP2 only, three responded and one had his tumor completely disappear, with no recurrence after 15 months of follow up. Describing his astonishment at this progression Krzysztof Wojkowski, a builder from London who was diagnosed with salivary gland cancer, recounted his experience:
“I was told there were no options left for me and I was receiving end of life care, it was devastating, so it was incredible to be given the chance to join the trial at The Royal Marsden, it was my final lifeline. I had injections every two weeks for five weeks which completely eradicated my cancer. I’ve been cancer free for two years now, it’s a true miracle, there is no other word to describe it. I’ve been able to work as a builder again and spend time with my family, there’s nothing I can’t do.”
Of the 30 participants given the combination therapy, seven responded to the treatment and six of these participants remained progression free after 14 months. Biopsies of the patients’ tumors before and after RP2 injections showed that the tumor microenvironment became significantly less hostile to immune cells. What’s more, the side effects of the treatment were very minimal, with the most serious reported effects requiring no medical assistance [3].
Commenting on the findings, study lead Kevin Harrington (ICR and RMNFT) concluded that, “our study shows that a genetically engineered, cancer-killing virus can deliver a one-two punch against tumors – directly destroying cancer cells from within while also calling in the immune system against them.”
Researchers like the team in Oregon will be eagerly observing the progress of this trial to see if the positive results keep coming as RP2 is tested in larger cohorts, giving more hope for the success of therapies like theirs that use a multiple target approach to combat cancer.