Targeting the mitochondria to attack drug-resistant cancer
A newly developed hybrid nanoparticle makes drug-resistant cancer cells vulnerable to chemotherapy.
Despite saving thousands of lives each year, chemotherapy often fails to prevent cancer recurrence in patients. One of the main reasons for this is that surviving cancer cells develop resistance to chemotherapy drugs similar to bacteria developing resistance to antibiotics. Now, a team of researchers collaborating across five different Universities led by Xiaoming He at the University of Maryland has found a way around this problem using a specially designed nanoparticle; when irradiated with near-infrared light, it makes drug-resistant cancer cells susceptible to chemotherapy.
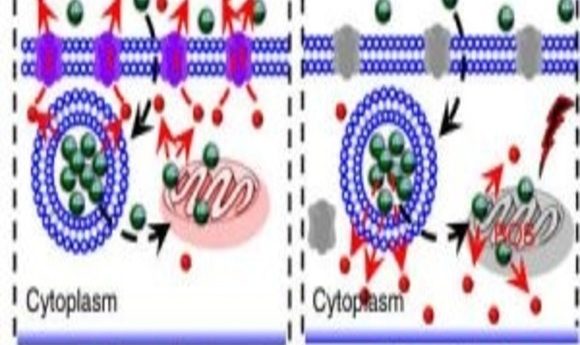
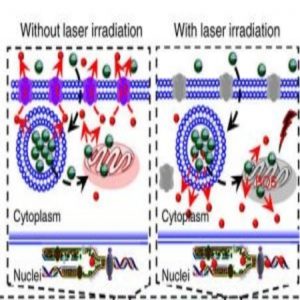
Many cancer cells avoid being killed by chemotherapy drugs by using molecular pumps located on their cell membranes. These proteins pump drugs out of the cell before they can enact damage, thus protecting the cancer cells. Since these pumps work against the concentration gradient, they require energy in the form of ATP to function.
“So, if we can cut off the energy supply of this pump, we should be able to minimize the function of the pump so that the cell can be less drug resistant,” said He. In order to achieve this, He and his colleagues decided to target the mitochondria, the major energy producing organelle in cells.
The researchers designed a nanoparticle with colloidal carbon and mesoporous silica to encapsulate drugs, and a lipid membrane coating to ensure stability for delivery into cancer cells. A pyruvate tag ensured that the particle reached the mitochondria. When irradiated with near-infrared laser light, the nanoparticles induced the formation of reactive oxygen species (ROS) in the mitochondria, which disrupted the electron transport chain and hampered the formation of ATP.
When He and his colleagues exposed cultured drug-resistant cancer cells to this nanoparticle and near-infrared light, it resulted in significantly fewer molecular pumps appearing in an active state. A simultaneously delivered chemotherapy drug–doxorubicin hydrochloride, paclitaxel, or irinotecan–induced much more cell death in irradiated cells than in controls.
In mice that had been grafted with drug-resistant tumors, administration of the nanoparticle coupled with near-infrared laser irradiation resulted in more chemotherapy drugs being taken up by the tumor cells and greater tumor shrinkage.
He believes that these nanoparticles can be combined with existing cancer treatments such as surgery to increase their efficacy in potential clinical applications. Matt Gottesman from the National Cancer Institute, who was not involved with this study, commented on the cleverness of this approach, suggesting that it may be used to attack many different ATP-dependent mechanisms of drug resistance, although precise targeting and applicability to different types of cancers may be challenges that need to be addressed before it can be clinically applied.
“So, is it the solution to drug resistance? No. That problem is far too complicated to solve this way. But it’s a clever new approach that could, under certain limited circumstances, (if you know where the tumor is, for example) be helpful,” said Gottesman.