Steadying your nerves: innovation for repairing peripheral nerve injuries
Hydrogel scaffolds can be used to guide mesenchymal stem cells derived from gingival tissue to develop into pro-regenerative cells, repairing peripheral nerve injury with the same effectiveness as an autograft.
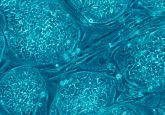
A cross-disciplinary team from the University of Pennsylvania School of Dental Medicine and Perelman School of Medicine (PA, USA) combined gingiva-derived mesenchymal stem cells (GMSCs) with a 3D collagen hydrogel scaffold to enable the functional recovery of nerves following peripheral nerve injury (PNI).
This innovative approach for guided nerve repair involved infusing a collagen hydrogel with human GMSCs to develop into neural crest stem-like cells (NCSCs) and Schwann precursor-like cells (SCPs). These cells are capable of migrating into natural nerve conduits, leading to the generation of functionalized neurons with the same effectiveness as the ‘gold standard autograft procedure.
However, nerve autograft causes injury in a previously uninjured body part, and nerve regrowth may not restore complete functionality. “Instead of an autograft, which causes unnecessary morbidity, we wanted to create a biological approach and use the regenerating ability of stem cells,” explained senior author Anh Le (University of Pennsylvania School of Dental Medicine). “To be able to recreate nerve cells in this way is really a new paradigm.”
The concept of GMSCs to treat PNIs built upon Le’s lab’s previous use of GMSCs in inflammatory diseases treatment and to regrow craniofacial tissue. Gingival tissue is an advantageous source of stem cells due to the ease of extraction and the tissue’s ability to heal rapidly after the procedure.
Utilizing commercially available scaffolds for nerve growth, the researchers introduced the GMSCs into collagen hydrogel. qRT-PCR analysis discovered significantly increased mRNA expression of a panel of 47 genes related to development of NCSCs and differentiation SCPs and genes associated with NOTCH3 signaling pathway activation.
“We observed this very interesting phenomenon,” says Le, “that when we changed that matrix density and suspended the cells three-dimensionally, they changed to have more neural crest properties, like Schwann cells.”
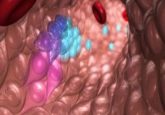
In vivo implantation of functionalized nerve conduits laden with GMSC-derived NCSC/SCP-like cells significantly improved the functional recovery and axonal regeneration in the segmental facial nerve defect model in rats. Additionally, the rats had improved facial palsy scores than those that received an “empty” graft and the implanted stem cells survived in the animals for months following the transplant.
 Can gold nanoparticles prevent nerve cell degeneration?
Can gold nanoparticles prevent nerve cell degeneration?
Researchers have recently designed and prepared gold nanoparticles for selective inhibition of extrasynaptic glutamate receptors, to prevent nerve cell damage and degeneration.
“The animals that received nerve conduits laden with the infused cells had a performance that matched the group that received an autograft for their repair,” commented D. Kacy Cullen (Perelman School of Medicine). “When you’re able to match the performance of the gold-standard procedure without a second surgery to acquire the autograft, that is definitely a technology to pursue further.”
Since the study focused on repairing small PNIs, there is still work to be done to evaluate the ability to repair larger injuries, such as those that result from oral cancer surgery. This would also provide the benefit of cosmetic improvements after repair from using the person’s own tissue to recover peripheral nerve function.
In future, the technique could be tested for repairing PNI in other parts of the body with the possibility of translation to clinical use.