Single-use plastics: are they safe?
In Life Sciences, new materials require new testing methods to ensure safety.
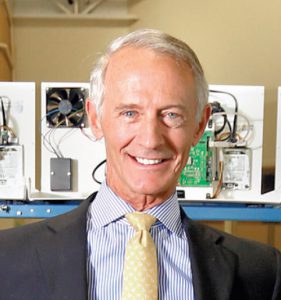
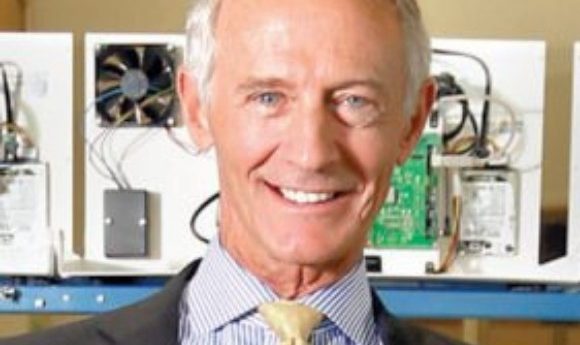
Kent Peterson has served as President and CEO of Fluid Imaging Technologies (ME, USA) since joining the company’s founder, Chris Sieracki, more than 15 years ago. Kent has served on many boards, is active in community affairs and was named Mainebiz Business Leader of the Year 2008. He is an honors graduate from Boston University’s Graduate School of Management (MA, USA) and a member of American Mensa Society.
Since initially visiting INTERPHEX years ago, I have observed a significant shift in focus of process components from steel and glass to plastic.
More specifically, ‘single-use’ or ‘solo-use’ plastic, which is never referred to by the politically incorrect moniker ‘disposable’ plastic, is the material of choice these days. There are many good reasons for this shift, including manpower savings from cleaning, to baseline sterility and lower initial investment.
The choice of whether to use plastic or glass depends on the intended application and understanding how the specific solution will interact with the container. There are advantages and disadvantages of each. Glass containers can have problems with breakage and delamination resulting in glass shards in the formulation. However, glass is transparent, which facilitates visual inspections. Plastic containers are lightweight, strong and can be handled easily. Additionally, plastic may be a better choice for certain solutions because, unlike glass, it will not demonstrate a marked change in pH over time.
New formulations on the market such as proteins and monoclonal antibodies have shown a higher sensitivity to silicone oil and aggregation from high particle counts, especially when exposed to physical stresses and agitation [1]. A recent study comparing the stability of prefilled syringes made of glass versus a plastic polymer demonstrate that the proteins were more stable after agitation in the plastic polymer syringes versus the glass [2].
Whilst I cannot weigh in on the cost-benefits relative to all the factors that have gone into this transformation (although I believe good cases have been made for this shift), I do wish to bring to mind a mostly overlooked aspect of using plastic single-use devices. From my experience in flow imaging testing, as well as a deeper understanding of studies relative to particulate matter in plastic, I believe that there is not enough education, discussion or documentation of micro- or nanoparticles contained in these plastic devices available to the provider or consumer.
Sub-visible dangers of plastic
A poster that was presented at the recent INTERPHEX conference contained an analysis of particulates in this vendor’s brand of tubing. I applaud their forthright disclosure of inherent particulate matter in their product. However, in discussing the details of the poster with the author, I learned that they relied upon USP 788 guidelines for particle bin sizing in microns. That’s a good start. Unfortunately, USP 788 was brought about years ago to control for particles that would cause capillary occlusion. In addition, it focuses on particles larger than 10 and 25µm. [3]
The general thinking in the public domain is that if the particles are smaller than 10 microns, they shouldn’t be a problem. This is true when the focus is on preventing capillary occlusion. What is now surfacing is the adverse impact of smaller particles causing immunogenetic responses to biologic drugs due to aggregation.
Sub-visible particle characterization is becoming a more important method for assessing drug substance and drug product stability. While current USP protocol does not require any characterization of particles below 10µm, it has been shown that submicron-sized particles can agglomerate during various stages of the post-production process. In one study, it was shown that nano- and microparticles were formed during the peristaltic pumping process. And, that during post-pumping agitation, there was a substantial increase in microparticle concentration coinciding with a significant depletion of the nanoparticle concentration, suggesting that agglomeration is the likely mechanism for larger microparticulate formation [4].
Elevating FDA regulations to the nano level
USP 788 acceptance criteria require the use of light obscuration and manual microscopy as methods to test for sub-visible particles in parenteral infusions. These two methods have also been adopted by many manufacturers to analyze particulates on medical devices. These routine methods only look to identify the count and concentration of larger particles (greater than 10µm). Fast forward to today. The same USP 788 protocols are still being followed despite the development of new technology that allows for the identification of particles smaller than that which was easily identifiable in the past, e.g. 10µm. Companies are slow to adopt change and will most often comply with the minimum requirements only.
Studies have shown that particles under 10µm can have disastrous consequences. For example, the FDA studied an approved biologic drug formulation that passed all the USP 788 required guidelines. Yet, upon public release, numerous cases of anaphylactic shock occurred and unfortunately, seven deaths [5]. The drug product was recalled.
Innovation ahead of regulation
Flow imaging technology is already available on the market for a more complete assessment of the nature and particulate load of biologic drugs. A USP Expert Committee has been convened and is at work to update USP 788 to include flow imaging as an orthogonal approach to complement light obscuration and manual microscopy. In fact, the FDA now recommends that flow imaging data and images be submitted with any new drug approval application.
While the FDA and USP acknowledge that flow imaging microscopy is useful down to a particle size of 2µm, newer still is an advanced form of flow imaging microscopy. It has been introduced to image and quantify particles down to about 300nm. What’s important to note is that the number of particles increase exponentially as one examines a smaller size spectrum. The technology is available to image and analyze particles in this size range. The morphological data are essential in the identification of particle or contaminant contained in the formulation.
Particulate contaminants are generally classified as one of three types. Extrinsic particles are not part of the formulation package or process and are foreign to the product. Examples include fibers, hair and plastic. Intrinsic particles arise from within the formulation or packaging processes, are generated from within the vial and are capable of change over time. Rubber from vial stoppers is an example of intrinsic contamination. Inherent particles are derived from the formulation itself, such as when a portion of it aggregates or crystallizes.
With the advent of new materials, such as plastic, envisioned to solve certain problems of the past, consideration should be given to the introduction of extrinsic and inherent particles to the formulation or production process. The potential effects of packaging component interactions are numerous. The presence of impurities can impact the potency of the drug product or result in changes to the formulations that create immunogenic results. Additional focus should be placed on the analysis of newer process materials used in the development and production of pharmaceutical products with the newer analysis techniques presently available for the long-term benefit of the end users.