Tau beats amyloid in top spot for predicting Alzheimer’s-associated neurodegeneration
Utilizing tau PET imaging, new research finds tau to be a more accurate indication for future neurodegeneration, highlighting its potential for precision medicine-based treatment approaches.
Amyloid-β has long been the bane of every Alzheimer’s researcher. Often found in large concentrations in the brain of Alzheimer’s disease patients, particularly in regions associated with Alzheimer’s symptomology, it seemed apparent that the protein was responsible for the debilitating neurodegenerative disorder. However, drugs against it didn’t work; drug trials that target amyloid-β are routinely being halted early and no novel Alzheimer’s drug has been brought to clinic since 2003.
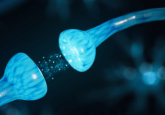
In that time, attention has turned away from the so-called amyloid hypothesis and researchers have shifted focus to the other big player in the Alzheimer’s brain: tau. In an afflicted brain, the tau protein becomes hyperphosphorylated, forming neurofibrillary tangles that create the pathology characteristic of Alzheimer’s disease.
The debate over the relative importance of amyloid vs tau in the development of Alzheimer’s has raged for years, historically with amyloid dominating research focus, yet new research from a collaboration between University of California, San Francisco (UCSF) and University of California, Berkley (both CA, USA) may have finally put tau on top.
“No one doubts that amyloid plays a role in Alzheimer’s disease, but more and more tau findings are beginning to shift how people think about what is actually driving the disease,” commented lead author Renaud La Joie (UCSF).
First thought to be impossible to measure in an in vivo brain, the development of an injectable molecule called flortaucipir – which can bind to tau tangles and emit a mild radioactive signal – opened up a new avenue for researchers as the protein could finally be identified in PET scans.
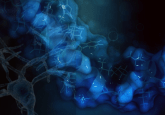
Utilizing the tau PET imaging technique, the UCSF team studied the relative distribution of tau tangles in a healthy brain and one of an individual with Alzheimer’s in an attempt to test whether levels of tau can be used to predict future neurodegeneration. Thirty-two patients were included in the study, each with early clinical-stage Alzheimer’s disease. Each participant received PET scans to measure the levels of amyloid and tau present in their brain, as well as an MRI to measure the brain’s structural integrity both at the launch of the study and at the follow-up visit an average of 15 months later
- Testing for tau: a new blood test for Alzheimer’s disease
- HSV1 and Alzheimer’s: The kiss of death
- A traumatic start to Alzheimer’s
Overall, the team found that levels of tau at the start of the study could predict how much neurodegeneration would occur during the subsequent months; local patterns of accumulation could predict later atrophy in that brain region with an accuracy of more than 40%. In contrast, amyloid buildup could only predict with an accuracy of 3%.
“Seeing that tau buildup predicts where degeneration will occur supports our hypothesis that tau is a key driver of neurodegeneration in Alzheimer’s disease,” explained La Joie.
It was notable that scans from younger participants had higher overall levels of tau in their brain, as well as a stronger correlation between the presence of tau and later atrophy, relative to older patients. The authors note that this may suggest that tau plays a greater role in early-onset Alzheimer’s, whereas additional factors, such as abnormal proteins or vascular injuries, have a larger effect in the development of the late-onset form of the disease.
The results of this study add to hopes of success for the tau-targeting drugs currently under development at UCSF and elsewhere. In addition, the application of the modified PET imaging technique may enable a more personalized approach to dementia treatment as clinicians are able to predict future neurodegeneration with a greater degree of accuracy than previously.
“One of the first things people want to know when they hear a diagnosis of Alzheimer’s disease is simply what the future holds for themselves or their loved ones,” commented UCSF lab-leader, Gil Rabinovici. “Now, for the first time, this tool could let us give patients a sense of what to expect by revealing the biological process underlying their disease.”
The team anticipates that the ability to predict future degeneration will allow clinical trials for novel Alzheimer’s treatments to assess whether or not the drug is actually altering the trajectory of the disease, something currently impossible due to the variation between patients. This would make it possible to adjust dosage where necessary or stop treatment all together if no benefit is occurring.
“Tau PET could be an extremely valuable precision medicine tool for future clinical trials,” Rabinovici concluded. “The ability to sensitively track tau accumulation in living patients would for the first time let clinical researchers seek out treatments that can slow down or even prevent the specific pattern of brain atrophy predicted for each patient.”