Back to basics with CRISPR
Base editing, a recent iteration of the CRISPR technique, has been demonstrated to cure cystic fibrosis in patient-derived stem cell-based intestinal organoids.
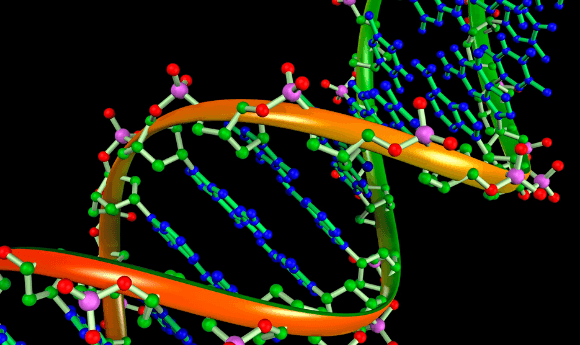
In its original format, the CRISPR—Cas9 genome editing tool cuts out a given genetic mutation and replaces it with the corrected gene. This version of the technique, called base editing, allows researchers to repair the mutation by directly converting one base pair to another, without ever cutting the DNA itself.
According to CRISPR researcher Maarten Geurts (Hubrecht Institute, Utrecht, The Netherlands), this base editing technique allows for greater precision than the standard Cas9 system and is less error prone, making it safer for patients were it to come to clinical use.
“With the traditional form of CRISPR—Cas, a certain piece of DNA is cut away, after which the cell has to repair itself, hopefully by replacing it with a ‘good’ piece of DNA that is made in the lab and presented to the cell,” explained Geurts. “With the new form of CRISPR—Cas, called base editing, the mistake in the DNA is identified, but not cut and replaced; it is repaired on site.”
In a recent study utilizing cystic fibrosis patient-derived intestinal organoids, Geurts and fellow researchers from Hubrecht Institute and UMC Utrecht (The Netherlands) have tested the base editing technique to see whether it can be applied in human stem cells and used to cure cystic fibrosis.
In cases of cystic fibrosis, a mutation in the CFTR gene results in a non-functioning protein, either due to the deletion of three nucleotides or a premature stop codon. Currently there is medication available for patients with the deletion mutation; however, for those with a premature stop codon there is no treatment. This is where base editing comes into play.
A prime time for genome editing
A novel genetic editing technique, prime editing, has been developed that improves on existing CRISPR—Cas9 techniques, producing higher precision and a wider selection of applications, potentially enabling researchers to correct 89% of established pathogenic genetic variants.
With the base editing technique, the researchers were able to identify the mutated CFTR gene and repair it, restoring the adenosine nucleotide back to a guanine without causing any further damage to the genome. This changes the codon to its functional triplet code and the cell can now produce a functioning CFTR protein.
Though promising in vitro results, the translatability of this research is unknown, and the researchers acknowledge the issue they will face in targeting delivery of the base editing treatment to the correct organ.
“This research represents a big step towards genetic repair of diseases in patients. However, a big question that remains is how to deliver the CRISPR-enzyme to the appropriate organs in the patient. Cystic fibrosis might also not be the most suitable disease to treat with CRISPR, as many organs are affected by the disease,” commented co-author Eyleen de Poel (UMC Utrecht).
Currently, therapeutic applications of CRISPR are showing promising clinical results, though many of these cases are in diseases where a single tissue or organ is affected, such as sickle cell anemia. Though further research is indeed required in order to bring the base editing technique into clinical use, the researchers hope that their recent study, published in Cell Stem Cell, will help in increasing understanding and the first clinical applications may be seen in as little as 5 years.