To cure or encourage: the paradoxical nature of an anti-fungal drug
A new study has uncovered how the presence of two genes may be responsible for the adverse effects sometimes caused by caspofungin, a drug used to treat a deadly fungal infection.
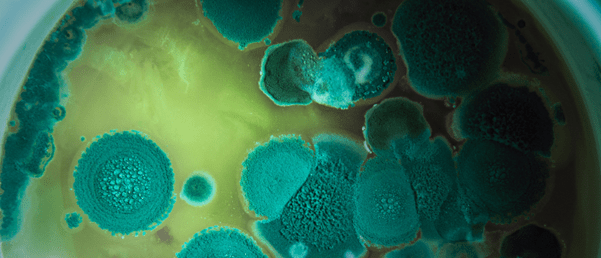
In a collaborative effort, researchers from Vanderbilt University (TN, USA), the University of Tennessee Science Health Center (TN, USA) and the University of São Paulo (Brazil), led by John Gibbons (University of Massachusetts Amherst; MA, USA), have identified two genes that may explain caspofungin’s inconsistent effects in the body. Used to treat sometimes deadly Aspergillus fumigatus (A. fumigatus) infections, this drug can cure, or occasionally encourage, the infection.
A. fumigatus is a fungus that doesn’t harm the average, healthy person. In fact, healthy people breathe in anywhere between 50 and 100 spores each day while outside; the body then identifies and destroys these spores, protecting the individual. However, when these spores are breathed in by someone who is severely immunocompromised as a result of cancer, COVID-19, HIV or other conditions, they can cause an infection with a 50% mortality rate and limited treatment options.
One of these treatment options is a drug called caspofungin. High doses of this drug have been known to occasionally have a negative effect, increasing fungal growth. This is called the caspofungin paradoxical effect (CPE).
 Researchers use CRISPR gene editing to uncover potential HIV treatments
Researchers use CRISPR gene editing to uncover potential HIV treatments
Using CRISPR researchers have identified 86 genes that could be associated with HIV replication and disease, opening doors to research on how the virus behaves in the body.
In their recent study, the researchers explored the molecular and genomic profiles of caspofungin-treated samples to determine how the CPE occurs. The research team sequenced the genome of 67 patient samples of A. fumigatus; half of these samples showed signs of CPE. They compared these two groups using genome-wide statistical analysis to determine how they differed genetically and how the genetic variants are associated with fungal growth at high doses of caspofungin.
They identified a list of genes that could play a role in causing the CPE. They then used CRISPR to delete the potential CPE-involved genes from the genome, allowing the researchers to narrow the list of genes down to two.
Gibbons reported, “It looks like there are many genes and many genetic variants that contribute to this phenotype. We aren’t done yet. One idea is that we could potentially generate new drug targets if we find the full collection of genes. We don’t understand the mechanisms yet.”
Further research is necessary to fully characterize how caspofungin works in the body, but this study serves as a strong base for the eventual development of a more comprehensive A. fumigatus treatment. The team hope to one day predict whether a patient will respond positively or negatively to caspofungin treatment based on their genotype, allowing doctors to make the right choice when it comes to treatment of A. fumigatus.