Novel method could lead to non-invasive diabetes monitoring

New research suggests that saliva could be utilized as a cheaper, pain-free alternative to blood for the monitoring of diabetes.
Diabetes affects approximately 425 million individuals globally; it is estimated that half of these cases are undiagnosed. The current standard for diabetes monitoring is blood glucose testing which can involve several finger-prick blood tests per day, potentially resulting in calluses and difficulty obtaining blood.
Regular monitoring of glucose levels is necessary to prevent hyper- and hypoglycemia, both of which can cause immediate and long-term complications in individuals with diabetes.
Now, in new research published in PLOS ONE, researchers have proposed the use of saliva as an alternative to blood testing. The work was led by Matthew Baker (University of Strathclyde, Glasgow, UK) in collaboration with researchers from the Federal University of Uberlandia (Brazil), the University of Vale do Paraíba (Sao Paolo, Brazil) and the University of Saskatchewan (Canada).
“Saliva reflects several physiological functions of the body, such as emotional, hormonal, nutritional and metabolic, and so its biomarkers could be an alternative to blood for robust early detection and monitoring. It is easy to collect, non-invasive, convenient to store and requires less handling than blood during clinical procedures, while also being environmentally efficient. It also contains analytes with real-time monitoring value which can be used to check a person’s condition,” explained Baker.
 Does COVID-19 pose a greater risk to individuals with diabetes?
Does COVID-19 pose a greater risk to individuals with diabetes?
Research relating to previous coronavirus outbreaks in combination with the available literature on SARS-CoV-2 has been utilized to explain why individuals with diabetes may have an increased risk of developing complications from COVID-19.
To test the utility of saliva for diabetes monitoring, samples were obtained from non-diabetic rats, diabetic rats and diabetic rats who had been treated with insulin.
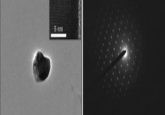
The samples were analyzed using attenuated total reflectance Fourier transform infrared (ATR-FTIR) spectroscopy, a technique that differentiates and identifies molecules based on their infrared absorption, without the need for potentially costly reagents. ATR-FTIR has previously been utilized in the detection and grading of brain tumors.
The team identified two biomarkers that had a strong correlation to glycemia and were able to differentiate between hyperglycemic and normal conditions. The two markers were utilized to distinguish between the non-diabetic, diabetic and insulin-treated diabetic rat models with 95.2% accuracy.
While additional research – including studies using human participants – are needed, it is hoped this novel approach could form the basis of a cost-effective, non-invasive approach to diabetes monitoring in both Type 1 and Type 2 patients.