The agony and ecstasy
The king of club drugs shows promise for treating post-traumatic stress disorder.
The story begins in Germany in 1912 in the Merck pharmaceutical laboratories, where researchers worked to develop a compound to control blood pressure. Unfortunately, a patent by rival company Bayer stood in their way. On the workaround path towards synthesizing a new compound, chemists produced an intermediary drug they called methylsafrylamin. The compound was only a precursor in the reaction, so it was archived with a cursory mention in the patent certificate.
In 1927, the year the original procedural patent expired, Merck researcher Max Oberlin investigated methylsafrylamin as part of a search for adrenaline-like compounds. Oberlin thought the drug was worth further investigation, but his research was halted due to a steep price increase. Methylsafrylamin returned to the archive, where it would wait another 40 years for Alexander Shulgin.
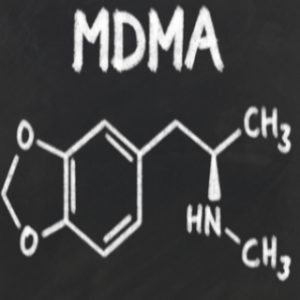
As an employee of Dow Chemical Company, Shulgin developed a new way to synthesize the compound, which he called 3,4-methylenedioxy- N-methylamphetamine, or MDMA; it is now known colloquially as “ecstasy.” He was the first to experiment with the drug in humans.
In his 1991 book PHIKAL (Phenethylamines I Have Known and Loved), Shulgin described witnessing the psychotherapeutic potential of MDMA in early experiments. Shulgin, a woman he called Janice, and her son, took 120 milligrams of MDMA each. The researcher, who was already experienced at taking and commenting on psychoactive drugs, observed and recorded MDMA’s effects in Janice.
It was now an hour into the experiment, and still no acknowledgment of any activity from the MDMA. Then, came the unexpected question, the “off the wall” question.
“Is it all right to be alive?”
“You bet your sweet ass it’s all right to be alive! It’s a grace to be alive!”
That was it. She plunged into the MDMA state, and started running down the hill, calling out that it was all right to be alive.
Janice explained to Shulgin that her mother had died while giving birth to her. For 50 years she had lived with the guilt. Shulgin wrote, “She had been in therapy with her family physician for about three years, largely addressing this problem, and apparently, what she needed was the acknowledgment that it was all right to be alive.”
Shulgin went on to study MDMA and numerous related compounds. He introduced friends and psychotherapists to MDMA as a psychotherapeutic aid. After publishing PHIKAL with his wife Anne, the couple went on to publish a second tome, THIKAL, which focused on another class of psychoactive compounds, the tryptamines. In 1994, the DEA raided his laboratory, forced him to turn over his DEA license, and condemned the Shulgins’ two volumes as cookbooks for illicit drug makers.
By this time, MDMA had become a popular drug with the electronic dance crowd that gathered at large, all-night, drug-fueled parties called “raves.” Multiple governments instituted laws banning not only MDMA, but many of its analogues as well. In the United States, MDMA was classified as a Schedule III substance, meaning it was considered by the FDA to have no medical value and a high potential for abuse.
Shulgin’s tale is a cautionary one: a researcher investigating the medical potential of a substance while it is gaining favor among a youthful subculture is stymied by governmental regulators who consider recreational drug use a greater risk to public health than any illnesses the drug might be able to treat.
MDMA is not the first instance of politics superseding public health in the case of psychoactive drugs. In 1973, President Richard Nixon instituted the War on Drugs, ostensibly to combat the wave of narcotics abuse among American youth. In fact, Nixon believed drug addiction to be a medical issue, not a criminal one. However, military veterans returning from Vietnam brought home not only opiate addictions but also vehement protests against the war as well. They began cohabiting with the hippie movement, organizing marches and other mass protests against the war and the sitting president. Nixon saw drugs as an opportunity to group addiction and its associated criminal behavior with the protest movement. The War on Drugs wasn’t just a public health policy; it was a political strategy to strengthen the government’s public image against growing anti-war sentiment.
The War on Drugs positioned the use of substances such as marijuana, LSD, and, later, MDMA, as public health crises. However, a new public health crisis is now on the rise: Combat veterans returning from Iraq and Afghanistan are bringing with them the remains of the hypervigilance they were forced to sustain in hostile territory. Reintroduction into non-military life has proved difficult and expensive; therapy for returning soldiers costs the US Department of Veterans Affairs over $1 billion a year, and the effectiveness of currently available treatments is questionable at best. So, researchers are once again turning to MDMA as a possible therapeutic tool.
Posttraumatic Stress is an Artifact of War
In 1973, Israel and Syria battled in the Golan Heights during the Yom Kippur War. An Israeli soldier, the story goes, was laying low to evade gunfire coming from the Syrians. His commanding officer ventured to stand. The soldier shouted, “Get down! They’ll kill you!” Moments later, a bullet hole appeared on the commander’s forehead.
The soldier had been calm and capable in the midst of the fighting. But upon his return home, he underwent a complete change. He was shell-shocked. He couldn’t sleep. He was always irritated. He obsessed over his inability to save his commander, a husband and father of three. The soldier wanted to go to his commander’s funeral, to pay his respects and tell the officer’s wife how he had died. But he could not gather the courage to go, which only added to the guilt he already felt over the man’s death.
The soldier began to use drugs. He abandoned his wife and two children, one of whom would go on to become a heroin addict.
This soldier’s daughter eventually sought treatment for her heroin addiction and ultimately trained to be a therapist. When she later reconnected with her father, she helped him discover that he was exhibiting the symptoms of posttraumatic stress. Soon after, the soldier came upon reports in the newspaper of a new research study involving a novel treatment for PTSD conducted by a former Israeli Defense Force psychiatrist, Sergio Marchevsky.
Marchevsky recounted the soldier’s story in 2009 from the spare interior of a low slung building in Be’er Ya’akov, about an hour outside of Tel Aviv, where he conducted an FDA-approved clinical trial to test if adding MDMA to talk therapy would help in treating PTSD. The drug was familiar in psychiatry and psychology circles due to its use in the 1970s as a therapeutic adjunct to marriage counseling, but its legal status had forced research into a holding pattern. Funds raised by several organizations in the United States, along with carefully written applications for research to the FDA, had finally opened the door for some researchers to use MDMA in new clinical trials. Marchevsky was one of a handful of psychiatrists across the globe trying to bring MDMA back into the psychotherapeutic fold.
MDMA and the Extinction of Fear
Posttraumatic stress disorder is a collection of symptoms resulting from the inability of the brain to dissociate fear from recollection of a traumatic, often life-threatening event. Treatment includes exposure therapy, in which the patient is prompted to revisit the traumatic memories in a safe environment. In the normal brain, exposure therapy stimulates the reduction of fear associated with memory in a process called fear extinction. In the brain of someone with PTSD, fear extinction does not occur.
MDMA may work as an adjunct to psychotherapy by stimulating fear extinction, said Ben Greenwood, a researcher at the University of Colorado. Greenwood studies the role of fear extinction in PTSD by observing changes in the brains of rats exposed to stressful conditions.
In a study published in 2015 in the journal Neurobiology of Learning and Behavior, Greenwood and his team hypothesized that exercise during a period of fear extinction in rats could reduce later fear relapses due to a mechanism involving the neurotransmitter dopamine, which is known to be sensitive to exercise.
Greenwood and his team employed a conditioned stimulus plus foot shock to create a fear response in rats, then removed the shock to instigate fear extinction. The team compared freezing behaviors in rats that ran on a wheel with rats that remained stationary. Then they froze the rat brains and performed in situ hybridization and mRNA analysis to learn how fear extinction and exercise interact.
Greenwood discovered that exercise reduced behaviors indicating the relapse of fear by comparing subjects that exercised during exposure to the conditioned stimulus in the absence of the foot shock, and those that did not exercise during the same type of exposure. After examining frozen brains of the subjects, Greenwood determined that exercise correlated with dopaminergic projections in the mesolimbic region of the brain.
“Dopamine modulates the activity of neuronal long-term potentiation,” said Greenwood, referring to one of the pathways by which the brain creates memories. This is where MDMA comes in. MDMA acts as an agonist at dopamine receptors, potentially modulating fear extinction for even longer relapse-free periods than exercise.
Additionally, said Greenwood, “MDMA might alter memory reconsolidation.” When traumatic memories are reconsolidated, they associate with more neutral emotions in place of the original fear. Thus, MDMA may be superior to exercise and other therapy adjuncts for PTSD.
“With current strategies, symptoms of fear return. Extinction doesn’t last. But with MDMA, symptom reduction lasts a long time, Greenwood said. To investigate precisely why, Greenwood is now developing a protocol to observe how MDMA changes neural architecture in rats so that he can develop a model to understand its effects in humans.
How MDMA affects the human brain is still a mystery. MDMA is a serotonin, norepinephrine, and dopamine agonist. The involvement of more neurotransmitters is not necessarily a good thing. “It’s such a dirty drug,” said Greenwood.
Dirty, not because of its reputation as a recreational drug but because it affects a broad range of receptor populations. For researchers trying to understand the neural basis of PTSD and its pharmacological remedies, specificity is critical.
Benzofurans and the Law
Small studies in several countries are currently investigating the efficacy of MDMA for treatment-resistant PTSD. However, the drug’s legal status hinders more widespread research. To find a workaround, in a paper published September 2016 in Naunyn-Schmiedeberg’s Archives of Pharmacology, Ezekiel Golan, and one group of researchers in Israel hypothesized that benzofuran analogs of MDMA, which are not illegal, may possess the same characteristics that make MDMA an effective adjunct to psychotherapy.
“Furan rings are significant pharmacologically,” said Golan, a chemoinformatician who advises on patent law for new chemical syntheses. “There are less hydrogens sticking off the ring, which makes the ring flat.” From a volumetric and electromagnetic perspective, he explained, it made the molecule look more like MDMA to the serotonin, dopamine, and norepinephrine receptors.
The researchers tested MDMA and 4 benzofuran analogues against 25 targets using radioligand, enzyme, and cellular receptor/transporter assays. They found that benzofuran compounds were as pharmacologically potent, or even more so, as MDMA, especially at the serotonin binding sites. And of particular interest for research purposes, they displayed a higher affinity for specific serotonin subreceptor populations, a finding that could have implications for future research seeking to correlate specific symptoms with specific receptors.
“From a legal point of view,” said Golan, “You cannot classify a chain of carbons, some of which have a single bond and others a double, as either an alkyl, alkene…” Golan explained that the benzofuran analogues were not included in the Schedule I listing of MDMA; thus, they remained legal for use in research and therapy.
Golan warns, however, that predicting a drug’s efficacy from an in vitro assay is impossible, and studying these kinds of drugs is especially challenging because it relies on subjects self-reporting about their hallucinogenic experiences. “It’s not even effective in animal models,” said Golan. “You can’t ask a rat or a pig or even a monkey what they felt.”
In the Pudding Lays the Proof
In 2009, in a bare white room in Be’er Ya’akov, Israel, a spool of tape spun on a black cassette machine. From speakers came the voice of the soldier, low and indecipherable in Hebrew. Sergio Marchevsky translated:
“Who is it I am seeking forgiveness from?” The soldier asks.
“There is no one who can give it to me,” he answers.
Marchevsky explained that this is a breakthrough. The soldier had never come to terms with his feelings of guilt and obsession over the death of his commanding officer. Then, under the influence of MDMA, and with gentle prodding by Marchevsky, the soldier confronted his memories and his emotions.
“I have to come to terms myself,” the soldier said, “I cannot continue with my life. The understanding will bring within itself acceptance and resignation. If not, my troubles will continue.”
“At least I see now what my psychological needs are. I have some introspection of myself. I understand for the first time the problem is inside and I have to find answers inside.”
Marchevsky ultimately stopped the trial to make what he called improvements to the study protocol, but the results were already exciting. Four out of five study participants who were diagnosed with chronic PTSD showed dramatic improvement using standard, symptom-reporting metrics. The fifth did not respond to the treatment. Marchevsky intends to restart the study soon.
The Long Strange Trip Goes On
Research into MDMA continues in multiple settings across the world, but challenges to its medical use have not abated. MDMA remains on Schedule I in the United States, and the FDA has no plans to move it anytime soon. Some countries, including the United Kingdom, have begun to place the benzofuran analogues under the same legal restrictions as MDMA.
In the meantime, PTSD continues its rise as the preeminent psychological condition afflicting war veterans, not to mention survivors of other tragedies. While law enforcement remains strictly against medicalization, there are plenty who believe the potential of MDMA demands further investigation.