Catching z’s to prevent heart disease

The association that sleep deprivation causes an increased risk of developing cardiovascular disease has been well established in scientific literature, but a detailed understanding of the pathophysiological link between the two had been lacking, until now.
Researchers from Massachusetts General Hospital (MA, USA), led by Filip Swiriski, have established a mechanism explaining how sleep deprivation causes an increased risk of developing heart disease. The team found that sleep deprivation increases the production of inflammatory immune cells as a result of the interruption of the regulation of the hormone hypocretin.
The research team split a cohort of mice with a genetic predisposition to develop atherosclerosis into two groups. The first group was subjected to interruptions in their sleep akin to those of someone waking due to noise or discomfort, while the second group was allowed to rest normally.
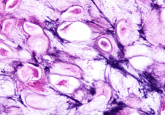
The sleep-deprived mice developed larger atherosclerotic plaques and were found to have higher concentrations of the inflammatory immune cell’s neutrophils and monocytes, which contribute to plaque formation, in their blood.
Further examination revealed that bone marrow-based production of inflammatory immune cell precursors in the sleep-deprived cohort was double that of the rested mice. This was found to be the result of the hormone hypocretin, which is produced in the hypothalamus and is closely associated with sleep regulation.
“We have discovered that sleep helps to regulate the production in the bone marrow of inflammatory cells and the health of blood vessels and that, conversely, sleep disruption breaks down control of inflammatory cell production, leading to more inflammation and more heart disease,” explained Swiriski.
Conducting further experiments on hypocretin deficient mice, Swiriski’s team established that hypocretin regulates neutrophil progenitors in the bone marrow. Without regulation by hypocretin, neutrophils release the signaling factor CSF-1, which in turn causes the proliferation of monocytes. Sleep deprivation of the mice leads to a decrease in hypocretin release, ultimately resulting in an increase in monocytes, which accelerated the development of atherosclerosis.
“This is a direct demonstration that hypocretin is also an important inflammatory mediator,” declared Swirski. “We now need to study this pathway in humans, explore additional mechanisms by which proper sleep maintains vascular health and further explore this newly identified neuro-immune axis.”