Sound the alarm: CD8+ regulatory-like T cells are first on the scene of a stroke
Researchers have demonstrated that a novel subset of immune cells provide protection against stroke in mice, potentially contributing to the development of human therapies in the future.
A team of immunologists and neurologists from the University of Pittsburgh (PA, USA) have identified a type of lymphocyte that provides immediate and long-lasting protection against ischemic stroke in mice. By understanding this immune response, researchers may be able to develop therapies based on this naturally evoked response to protect those at risk of stroke.
An ischemic stroke occurs when a blood clot forms, blocking the movement of blood and oxygen to the brain. It is the most common type of stroke, affecting 800,000 Americans every year. However, there are only two available stroke treatments, both of which must be administered soon after stroke onset. These treatments, then, are not accessible to all 800,000 Americans, let alone stroke survivors in other parts of the world. Therefore, an alternative therapy is necessary.
 Why do some T cells stay in the gut?
Why do some T cells stay in the gut?
Researchers uncover how epithelial cells and T cells communicate to find out why intraepithelial T cells stay patrolling the intestines.
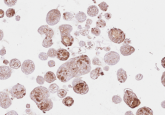
The current study modelled stroke in mice, investigating naturally occurring responses to stroke onset. They used numerous techniques, such as immunohistochemistry, image analysis, flow cytometry, magnetic resonance imaging and real-time PCR to detect and identify the molecular basis of the post-stroke response.
Researchers found that a subset of CD8+ regulatory-like T cells (CD8+ TRLs) are signaled by dying brain cells, within 24 hours of the clot forming, to the brain. Once in the brain, the immune cells release neuroprotective molecules that reduce inflammation.
“The beauty of CD8+ TRLs is in their fast response. They confer very potent protection to the brain, which can last a long time,” reported co-corresponding author Xiaoming Hu. “Most importantly, these cells are easily accessible because they circulate in the blood before they enter the injured brain.”
Researchers also demonstrated that mouse brain inflammation following a stroke was greater when CD8+ TRLs were artificially depleted in the blood versus normal counts of CD8+ TRLs. Additionally, mice who had their CD8+ TRLs levels artificially boosted after a stroke recovered more quickly and had less severe symptoms than mice who were left untreated.
Harnessing the effects of these naturally occurring immune cells in response to clot formation may lend itself to the development of effective stroke treatments in the future. The results demonstrated in mice provide an important basis for stroke research and potential human intervention.
Co-senior author Jun Chen suggested, “Creating shelf-stable and ready-to-use CD8+ TRLs or developing a cocktail of neuroprotective signaling molecules released by those cells once they reach the brain could present effective future therapies against stroke and offer hope to hundreds of thousands of patients who are ineligible for treatments available to them currently.”