Who won the 2025 Nobel Prize for Physiology or Medicine?
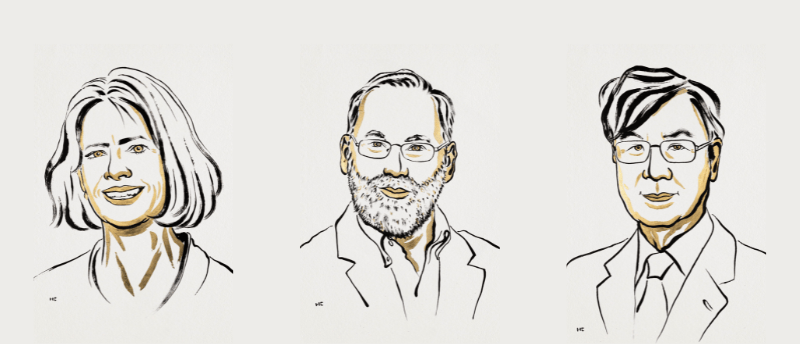
The discovery and characterization of regulatory T cells has been selected as Nobel Prize winning research, with three researchers selected to share the prize. Mary Brunkow (Institute for Systems Biology, WA, USA), Fred Ramsdell (Sonoma Biotherapeutics, CA, USA) and Shimon Sakaguchi (Osaka University, Osaka, Japan) have been awarded the Nobel Prize in Physiology or Medicine 2025 for their discoveries concerning regulatory T cells (Tregs) and the genetic factors that underlie peripheral immune tolerance, which prevents the immune system from harming the body. Going against the flow In the ever-evolving arms race between pathogens and the immune system, some pathogens have evolved...
To view this content, please register now for access
Join our member community for FREE to access a collection of journal and online-only features, including:
- Exclusive access to educational videos, eBooks and insights into top BioTechniques journal articles
- The latest news and journal updates delivered straight to your inbox when you want it
- Personalized recommendations for the latest member-exclusive podcasts, interviews and expert opinions
- Priority registration to webinars, panel discussions and events
- Access to competitions and journal publication discounts, including 10% off open access fees when you sign up today!