Connecting the dots between HPV, the vaginal microbiome and race

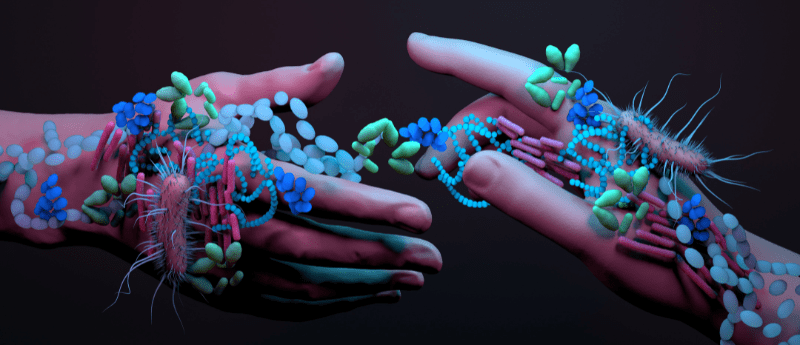
 The vaginal microbiome is a dynamic ecosystem that is constantly changing, influenced by various factors including menstrual cycles, sex and diet; but how do lived experiences, such as racism, impact the vaginal microbiome? And what effect does this have on HPV-related oncogenesis?
The vaginal microbiome is a dynamic ecosystem that is constantly changing, influenced by various factors including menstrual cycles, sex and diet; but how do lived experiences, such as racism, impact the vaginal microbiome? And what effect does this have on HPV-related oncogenesis?
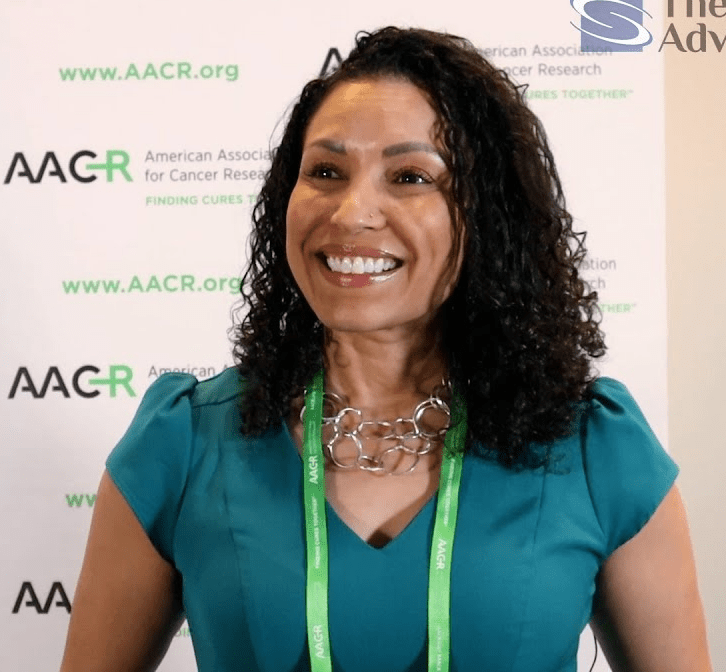
We spoke to Kathy Tossas (left), an assistant professor at the Virginia Commonwealth University School of Medicine (VA, USA) and Director of the Catchment Area Data Access and Alignment initiatives at the Massey Cancer Center (VA, USA), whose research aims to answer this question.
HPV is a common virus in humans that can often cause symptomless infections, the majority of which resolve within 2 years without medical intervention. However, in some cases, HPV can cause precancerous lesions, which, if not removed, increase the risk of cancer in the affected area. One area that can be affected by HPV is the cervix: HPV is the primary cause of cervical cancer. The development of an effective vaccine and screening strategy means that cervical cancer is largely preventable and has the potential to be eradicated; however, we still see women around the world dying of cervical cancer. This is a failing that Kathy sees as an issue of social and reproductive justice, further motivating her work in this critical field.
The role of the vaginal microbiome
Just as the gut microbiome plays an important role in gut health, the vaginal microbiome is a critical determinant of vaginal health. However, unlike the gut, having diverse microbial taxa in the vagina is detrimental, not beneficial, to health. The vaginal microbiota is dominated by Lactobacillus, a genus of bacteria that has antimicrobial properties, protecting the space from pathogens like HPV and preventing infections such as bacterial vaginosis. “A more diverse microbiome in the vaginal space is not a good thing because higher microbial diversity is associated with higher inflammation in the vaginal space, which can cause damage to the tissues,” Kathy explains. Therefore, a more diverse vaginal microbiome can allow HPV to thrive, further disrupting its composition and increasing the risk of precancerous lesions and cervical cancer.
“The vaginal microbiome is also racially differentiated. Black women are more likely to have more diverse vaginal microbiomes than White women, who are more likely to have homogeneous microbiomes that are Lactobacillus dominant.” To better understand this and the impact this has on HPV-related oncogenesis, Kathy looked at samples from a large and diverse group of women, generating a robust data set to analyze. She found that the vaginal microbiome was differentially impacting the risk of precancerous lesions. Among White women, those with a more homogenous microbiome had a significantly lower risk of developing precancerous lesions than those with a more diverse microbiome. In contrast, Black women had an increased risk of precancerous lesions, regardless of their microbiome diversity. In fact, when comparing White women with homogenous microbiomes to Black women with homogenous microbiomes, they found that Black women were at almost eight times greater risk of precancerous lesions.
“This shows that there may be a different etiology, or different mechanisms through which, in this case, HPV leads to pre-cervical cancer in Black versus White women. It may be that the vaginal microbiome plays a stronger (perhaps protective) role in White women than Black women,” hypothesizes Kathy.
 Talking Techniques | Microbiome profiling techniques: from immunology to agriculture
Talking Techniques | Microbiome profiling techniques: from immunology to agriculture
Here, we explore microbiomes and the techniques used to profile them. Get an overview of each techniques’ working principles, their pros and cons and the different applications that they are best suited to.
Getting to the root
One explanation for this increased risk of lesions among Black women could be low-level chronic inflammation. “Black women are known to have low-level chronic inflammation all the time. A lot of this is the result of their structural experiences, including racism, discrimination and micro–macro aggressions.” As the microbiome is immunomodulatory, in normal circumstances if there’s a stimulus your microbiome changes and your immune system responds; however, if the immune system is already heightened, there may be no immune response because it is already taxed. “I have a feeling that that may be what is occurring biologically in Black women: that they have a higher risk of developing a lesion regardless of their microbiome because they are already under this heightened state of inflammation.”
Another avenue of research Kathy is exploring is HPV heterogeneity. There are over 200 different types of HPV virus, categorized as either carcinogenic and high risk, or low risk. However, Kathy believes it may not be as simple as either high risk or low risk and to explore this avenue further, she is investigating the L1 gene, which encodes HPV’s viral capsid and is important in vaccinology.
Moving forward
The microbiome is a growing field of research, with people investigating various aspects, including treatment response and the use of the microbiome as a biomarker. This could prove useful in cervical cancer screening programs – as HPV is such a common virus, many people are HPV positive when they have their cervical screening and are therefore required to have a biopsy. However, for around every 1600 biopsies carried out, just one case of cervical cancer is diagnosed. Cervix biopsies carry risks such as cervical insufficiency, cervical scarring, bleeding, pain and pre-term birth. For Kathy, a change in the status quo is required, “I think it’s time for us to rethink cervical cancer screenings and how we treat the cervix. This research could help determine if the microbiome could be used as an additional data point for clinicians to decide whether or not a biopsy is needed.”
Kathy believes that the key to understanding the role of race and racism in cervical cancer risk and the vaginal microbiome is transdisciplinary research and collaboration. The vaginal microbiome, HPV viral load, the immune response and cervical cancer risk are all connected and influence each other, in what Kathy calls an ‘interactome’. Central to this interactome is stress, which we know is differential by race. Drawing data and expertise from other fields, such as behavioral science, as Kathy is doing in one project, can help understand these connections.
When asked what her one wish for her research would be, Kathy reiterated inter- and transdisciplinary collaboration and the joining of data. “As well as ensuring our research is comparable and reproducible, large data sets create much more power for us to detect differences that can actually lead to something.”
The cervical cancer landscape has changed drastically in the past few decades. “Right now, cervical cancer is no longer a death sentence. In fact, it is the only cancer considered eradicable by the World Health Organization.” An issue close to her heart, Kathy’s mother was diagnosed with cervical cancer in the 1980s, with the only treatment option available being a radical hysterectomy. “My mom wanted to have more children, but she wasn’t able to. Well, no longer do women have to deal with those consequences. We have significantly reduced cervical cancer incidence and mortality particularly in the US due to effective screening and HPV vaccination. Now, let’s focus on reducing morbidity by learning how to intercept pre-cancerous lesions before they turn into cancer. There is still room for improvement!”