Monocytes: an important piece of the Zika microcephaly puzzle
A new study sheds light on the connection between Zika virus infection and microcephaly, identifying a cell that acts as a Trojan horse by carrying the virus to the developing fetus.
Zika is one of the most puzzling viruses in recent human history. Although it was identified in 1947, it didn’t become a public health emergency until 2016 when researchers linked it to microcephaly in babies born to infected pregnant women. Scientists still don’t know why and how Zika virus causes these birth defects.
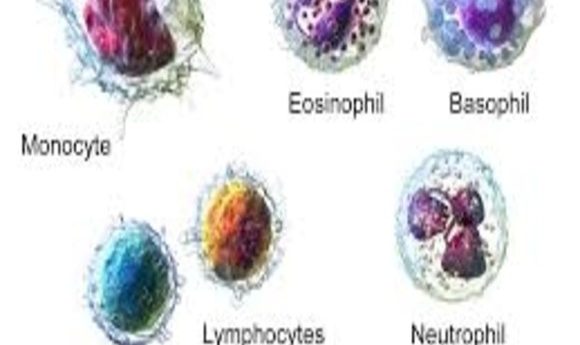
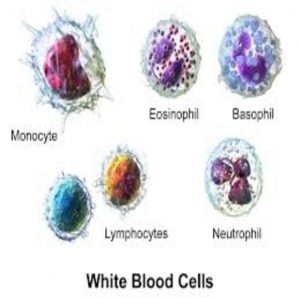
One of the most bewildering questions is how the virus crosses the placenta—an immunologically sheltered space in the human body—to affect the developing fetus. A new study published in Nature Microbiology now shows that CD14+CD16+ monocytes are the main target of Zika virus and that these cells help carry the virus across the placenta (1).
“We started this study right at the beginning of the current Zika epidemic. We wanted to know what happens during the first few days after infection and if the blood cells carry the virus to the placenta. Luckily, we also had access to samples from patients at the very early stage of infection,” said Daniela Michlmayr from the University of California, Berkeley, lead author of the study.
Michlmayr and her colleagues collected peripheral blood mononuclear cells (PBMCs), circulating blood cells consisting of lymphocytes and monocytes, from healthy donors. They infected the cells with Zika virus and then compared the numbers of different cell types between infected and uninfected PBMCs. They found significantly more CD14+CD16+ monocytes in infected PBMCs compared to uninfected PBMCs.
The team next stained infected PBMCs with an antibody that labeled Zika virus proteins to find out if the virus was replicating inside the cells and, if so, which cells permitted replication. They noted that approximately 6% of live PBMCs actively carried the virus, and approximately 80% of those Zika virus–containing PBMCs were monocytes—mainly CD14+CD16+ cells. Previous studies exploring other viruses indicated that monocytes can disseminate viruses to other body parts, including across the blood–brain barrier and other immunologically sheltered spaces, potentially crossing the placenta to reach a developing fetus.
Michlmayr’s team next collected PBMCs from 29 Zika virus infected patients during acute illness who were enrolled in a pediatric study in Managua, Nicaragua. When they stained these cells to label Zika virus proteins, the results mirrored those of their previous experiments. In addition, they also observed an increase in the CD14+CD16+ monocyte population 24h to 48h post-infection.
“We are very excited to characterize this first stage of Zika [virus infection],” said Michlmayr. “We believe that these infected monocytes will work as Trojan horses. If we are somehow able to stop these infected monocytes from going to the placenta, we might be able to prevent any harm to the fetus.“