Photo feature: Seeing malaria in the Asia-Pacific
My journey to document the face of malaria began with a project initiated by Professor J. Kevin Baird, from the Oxford Clinical Research Unit (Vietnam) to raise awareness of this disease across the Asia Pacific. Our project is part of the public engagement section of the Oxford University Clinical Research Unit. From the perspective of public awareness, malaria in the Asia-Pacific is virtually invisible as it is generally seen as an African problem. The goal of our project ‘Seeing Malaria in the Asia-Pacific’ is to correct the incorrect view of the suffering caused by endemic malaria.
Over the past few years this project has allowed me to travel to diverse, isolated regions of the Asia Pacific where malaria remains part of the daily life-experience of millions of people. These experiences have shown me that people who live with malaria in the Asia Pacific are the least ‘visible’ as the disease is found in areas of poverty and isolation. These people are ‘voiceless’.
My mission is to capture and communicate the ‘human faces’ of the Asia-Pacific malaria problem to audiences unfamiliar with it. My goal in taking the images was to faithfully capture the daily life, sufferings and humanity of people living with malaria, which otherwise is largely invisible to the rest of the world. We hope to elevate awareness of this serious Asia-Pacific health problem. It is important to help people across the world see beyond the invisibility of these isolated and impoverished communities in Asia-Pacific and give them their rightful places.
Prof J. Kevin Baird, Head of Eijkman Oxford Clinical Research Unit, Jakarta (Indonesia) has pointed out that malaria in Asia is a very different problem than malaria in Africa. Different species of mosquitoes are involved in transmission of malaria in Africa and Asia. In addition, malaria is caused by a different strain of the malaria parasite; in Africa most malaria patients are infected with Plasmodium falciparum, and while P. falciparum also exists in Asia, about half of the malaria cases are caused by a different strain: Plasmodium vivax . Vivax malaria is transmitted differently and so it affects communities differently. In Asia many people do not have adequate access to diagnostic services and treatments, and this makes the problem of malaria more widespread. On top of all this, P. vivax malaria is difficult to treat: the main drug used in clinics, primaquine, is dangerous for the 8% of people in South and Southeast Asia who have an inherited abnormality called G6PD deficiency.
Malaria represents an enormous and complex burden in South and Southeast Asia, and yet our region only receives a small fraction of the global funding for malaria control and elimination: of the US $2.7 billion invested in 2016 – only 7% was pegged for efforts in South and Southeast Asia. The increased awareness of malaria in Asia will benefit a more balanced funding for the Asian communities as we need better tools and research in working towards realizing the 2030 elimination date.
We hope that the collection of photographs will raise awareness of the malaria burden suffered by the inhabitants of these remote communities. This project humbles me. In many of the places I visited, government healthcare amenities are severely limited. Malaria patients often had to travel long distances to get the medical attention they required. For someone from a first world country, it is almost unthinkable to imagine the basic need for medical care which was lacking for so many people in this part of the world. I am proud to be associated with this non-profit project. Such documentation is important as it shows the world the need to continue to support the efforts to attain a ‘malaria-free world’.

Rani lives with her grandma and family in the border of Timor and Indonesia. Her parents had left the countryside to work in urban Jakarta leaving the children alone with their old grandma. Poor living conditions contribute to endemic malaria, which is more frequently found in the isolated rural areas in Asia Pacific. One approach has been to provide ‘long lasting insecticide-treated bed nets’, which are a form of personal protection that have been shown to reduce malaria illness in many different areas around the world. Bed nets act as a barrier against the bites of a range of species of malaria-carrying mosquitoes. Although bed nets are not effective in all areas suffering from malaria infection, where this simple preventative measure is effective then it can be a very cost-effective public health measure.
Photo credit to Pearl Gan in association with Oxford University Clinical Research Unit, Vietnam and EOCRU Jakarta.

This student from a high school in the Bandarban district in Bangladesh is showing her BRAC Malaria Progress Card to us. The card shows the date that she was initially found to have malaria and her health progress. According to the Principal, usually the students contract malaria in their hometowns during the school holidays. Their homes in the outback regions required them to travel for a few days before they are able to reach home.
According to the National Malaria Elimination Programme (NECP), currently 93% of the country’s 29,247 malaria cases are from the Chittagong region. The major reasons are their hilly frontiers, profuse rain, large forest area, inadequacies in healthcare system and problems faced while reaching treatment and other healthcare service.
Photo credit to Pearl Gan in association with Oxford University Clinical Research Unit, Vietnam and EOCRU Jakarta.
[column size=”1/2″]

When patients attend the Mebung Health Centre in Alor Island (Indonesia) they often travel long distances and are accompanied by their family members. In many cases the families face reduced income and hardship to make the long journey to receive treatment. Usually people in the island only seek medical help when they have exhausted help from their traditional medicines and bomohs, sometimes risking their own health. This photo shows the husband of a patient with fever and nausea being interviewed by the EOCRU staff, Ms Lenny Ekawati, who was obtaining consent from the patient’s husband.
Photo credit to Pearl Gan in association with Oxford University Clinical Research Unit, Vietnam and EOCRU Jakarta.
[column size=”1/2″]

This photo is taken in the Bandarban track. The headquarter of the 69th Infantry Brigade of Bangladesh Army is stationed here. It is one of five cantonment in Chittagong Hill Tracts area. Special permission has to be granted to enter this region.
Volunteer staff form the backbone of malaria control efforts in BRAC’s malaria program in outback Bangladesh. They are usually local residents recruited and trained by the BRAC’s malaria control program. In most of malaria-endemic Asia-Pacific, patients must find their way to such services.
Photo credit to Pearl Gan in association with Oxford University Clinical Research Unit, Vietnam and EOCRU Jakarta.

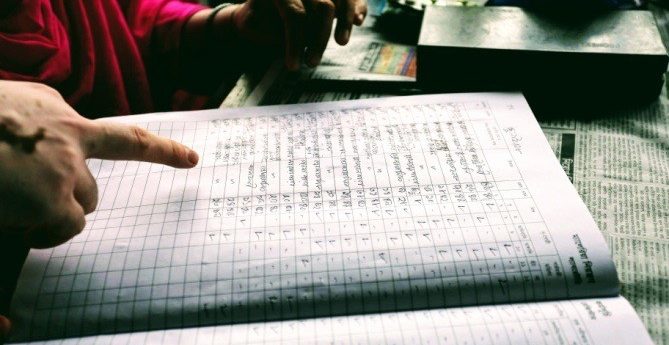
The results from the analysis of a patient’s blood sample are recorded in Bangladesh Rehabilitation Assistance Committee’s BRAC Malaria diagnosis logbook in a suburban outback of Bandarban district in Bangledesh. This logbook serves as a crude surveillance tool that allows the staff to estimate the percentage of febrile patients who were subsequently shown to be infected by malaria versus the many other causes of fever.
Photo credit to Pearl Gan in association with Oxford University Clinical Research Unit, Vietnam and EOCRU Jakarta.

This photo shows a staff member from the Shoklo Malaria Research Unit patiently recording the patient’s details in the patient’s logbook. Shoklo Malaria Research Unit (SMRU) is a field station of the faculty of Tropical Medicine, Mahidol University, Bangkok, Thailand, and is part of the Mahidol-Oxford Research Unit (MORU) supported by the Wellcome Trust (UK). The main objective of SMRU is to provide quality health care to the marginalized populations living on both sides of the Thai–Myanmar border in the Mae Sot area, Tak Province. This is achieved by research and humanitarian services, with an emphasis on maternal–child health and infectious diseases.
Photo credit to Pearl Gan in association with Oxford University Clinical Research Unit, Vietnam and EOCRU Jakarta.

The results from the analysis of a patient’s blood sample are recorded in the diagnosis logbook in a suburban outback region of Bandarban, Bangledesh. This logbook serves as a crude surveillance tool that allows the staff to estimate the percentage of febrile patients who were subsequently shown to be infected by malaria versus the many other causes of fever.
Photo credit to Pearl Gan in association with Oxford University Clinical Research Unit, Vietnam and EOCRU Jakarta.

The Bandarban District of in South-Eastern Bangladesh is known to be endemic for malaria due to Plasmodium falciparum. This photo depicts a Bangladeshi woman in her home in the Bandarban district. The improvised housing in this area renders them porous to mosquitoes carrying the endemic malaria parasite, a common problem in many rural areas in the Asia-Pacific. Villagers in this district are monitored by BRAC’s Malaria Program, which sends their local volunteers to provide malaria testing services to the villagers in the area. However, due to the remoteness of the location the analysis and reporting of test results many take days or weeks.
Photo credit to Pearl Gan in association with Oxford University Clinical Research Unit, Vietnam and EOCRU Jakarta.
See more of Pearl’s work at: www.pearlgan.com
You might also like: