Beta-blocking cancer
Beta blockers treat high blood pressure, but that’s not stopping researchers from repurposing them for use in the war against cancer.
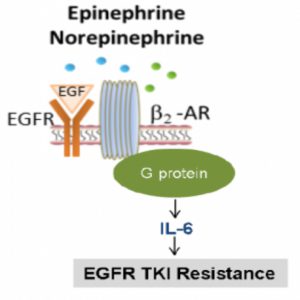
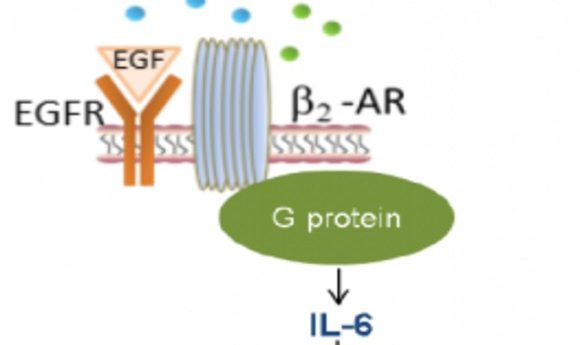
Diagram of the proposed EGFR signaling mechanism
Credit:Monique Nilsson, PhD
Epidermal growth factor receptor (EGFR) mutations are common in patients with non-small cell lung cancer (NSCLC), so patients regularly receive EGFR inhibitor treatment. Unfortunately, 50-80% of EGFR treated patients develop resistance to this treatment, resulting in a poor prognosis. Clinical scientists at the University of Texas Anderson Cancer Center have discovered that beta-blockers could be used to block EGFR resistance in NSCLC patients. They published these results in Science Translational Medicine.
“The results are very exciting for us because this opens up the possibility that EGFR mutant patients may get a lot more benefit [from EGFR inhibitors] by just adding this inexpensive and well tolerated type of drug [beta-blockers],” said study lead John Heymach.
Surges in the immune protein interleukin 6 (IL-6) have been linked to EGFR resistance and the scientists suspected that stress hormones, such as adrenaline, might regulate IL-6. Therefore they set out to investigate the interaction between stress pathways and NSCLC.
The scientists found that EGFR-resistant NSCLC cells had heightened adrenaline signaling and that this was associated with high IL-6 in both cell line and mouse experiments. Digging further into the mechanism, the scientists revealed that stress hormones promoted IL-6 transcription via beta-adrenergic receptor stimulation.
Beta-blockers effectively block beta-adrenergic receptors and are traditionally prescribed to reduce blood pressure. “Given how frequently lung cancer patients are under major stress, this [result] gave us pause to see the impact stress had on making these cancers grow faster,” said Heymach.
When applied to EGFR-resistant cell lines and rodent tumors, beta-blockers prevented tumor growth and improved the response to EGFR treatment. Upon retrospectively examining NSCLC clinical trials, Heymach and his colleagues were excited to find that patients using beta-blockers benefited more from EGFR inhibitor treatment.
“I thought the combination of experimental investigation and clinical data was very valuable,” said Hildegard Schuller from the University of Tennessee, who was not involved with the study. Schuller pointed out that other clinicians are now examining potential beta-blocker benefits for a variety of adenocarcinomas.
Heymach is now planning a randomized prospective study to definitively ascertain whether beta-blockers will benefit EGFR-resistant NSCLC patients.
“The only caveat is that when you use [beta blockers] for a long time, they can sensitize the beta-adrenergic receptors to respond to stress hormones at much lower concentrations than normal. There is the potential that the beta blockers can turn into a tumor promoter instead of an inhibitor,” said Schuller. “So in prospective studies, the patients need to be monitored.”