Binge eating? Blame the brain

Researchers have found that triggering a special part of the brain induces binge eating behavior in mice. Will this lead to treatments to prevent overeating?

A mouse binge-eats a chocolate chip cookie.
Credit: Anthony Van den Pol, Yale University
Every once in a while, there is that box of cookies that no-one can resist, even after a full meal. For some people though, frequent overeating despite being full is a regular issue beyond their control—a binge eating disorder. In a recent study reported in Science, researchers from Yale University zeroed in on one of the parts of the brain that triggers binge eating behavior in mice [1].
Anthony Van den Pol, who led this study, is a professor of neurosurgery at Yale University. He knew from previous studies that patients receiving deep brain stimulation for treatment of movement-related disorders occasionally experienced binge eating as a side effect. Intrigued by this phenomenon, he and his colleague, Xiaobing Zhang, decided to seize this opportunity to see if they could discover the exact part of the brain involved in binge eating disorder. Based on anatomy and preliminary food-intake experiments in mice, Van den Pol and Zhang narrowed down their search to gamma-aminobutyric acid (GABA)-secreting neurons in the zona incerta region of the brain.
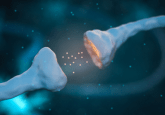
For their new study, the researchers genetically modified mice such that their GABA neurons could be stimulated by blue light to fire an impulse. “The animals remarkably ran over to the food and started eating [on stimulation with light], and when we turned the light off, they stopped eating,” Van den Pol said. “Even if they were not hungry, they began eating!”
Interestingly, the mice started eating within 2–3 seconds after the researchers stimulated their GABA neurons. This response time was much faster than the response time of about 6 minutes that was recorded in a study of another brain region that influences food intake [2]. “We were surprised that we got such reliable and fast eating response. It was unexpected,” said Van den Pol.
Next, the team tested the long-term effects of GABA neuron stimulation on food intake in mice. They stimulated the mice for a few minutes intermittently each day over a period of 2 weeks and noted that the mice ate more and gained weight over time. Conversely, when mice were genetically induced to produce caspase in the GABA cells, which kills the cells, they ate less and their body weight decreased over the long term.
“It’s pretty exciting to be able to pinpoint an actual circuitry involved in rapid binge-like eating behavior,” said Traci Czyzyk, an assistant professor at the College of Medicine, Pennsylvania State University, who was not involved in this work. She believes that this finding will encourage researchers to consider GABA neurons in their studies, in addition to the usually studied reward pathways.
Mice and humans may have similar pathways involved in binge eating, but stimulating specific neurons in humans would not be as simple. “This is kind of an invasive procedure,” said Czyzyk, adding that people might be skeptical of undergoing neural surgery for treating binge eating disorder. Van den Pol agrees that developing drugs that selectively activate or inhibit these cells might be more feasible than neural stimulation for controlling food intake in patients in the future.