Universal CAR-T: taking on relapsed/refractory T-cell acute lymphoblastic leukemia
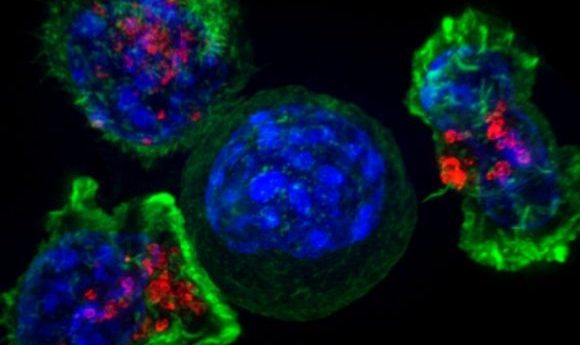
A new study has shown initial success of a novel universal CAR-T therapy where previous attempts have failed – in the treatment of T-cell acute lymphoblastic leukemia.
A current clinical safety and efficacy study, conducted by a Chinese research collaboration, has demonstrated the first-in-human application of universal CAR-T therapy for relapsed/refractory T-cell acute lymphoblastic leukemia (r/r T-ALL). The results of the trial are due to be presented at the AACR Virtual Annual Meeting I (27–28 April 2020).
The team set out to address some of the key issues in r/r T-ALL treatment, such as the high relapse rate and poor progression of CAR-T therapies for this disease, due, in part, to the contamination of the therapeutic cells with malignant T-cells and the shared common surface antigens between the opposing cell types.
To do this, they designed a universal CAR-T platform called TruUCARÔ GC027; incorporating a second-generation CAR that had been developed using CRISPR technology to disrupt the TCRα and CD7 regions of the receptor, preventing the occurrence of graft vs host disease and the targeting of existing healthy T-cells in the body.
Advances in cell engineering therapies: where are we in 2020?
Cell engineering as a field has developed rapidly in recent decades and is now entering therapeutic applications, but which are the key areas to watch in 2020?
Anti-leukemic efficacy and expansion were first monitored in a T-ALL xenograft murine model, before the current human trial to establish safety, efficacy and expansion kinetics was initiated. This human trial currently has five participants between the ages of 19–38, with a diverse range of marrow tumor load from 4–80.2%.
Each patient received a 6-day preconditioning treatment of chemotherapy prior to their single infusion of GC027 at a dosage range between 0.6–1.5×107/kg. At the initial follow-up for the study at day 28 post infusion, four of the five patients observed minimal-residual-disease negative complete responses (MRD-CR). This response was observed in three of these patients at later follow-ups between 61–161 days later with the fourth yet to have their follow up.
The peak expansion of the GC027 cells was measured in all MRD-CR participants between weeks 1–2. Adverse events of cytokine release syndrome were recorded at Grades 3 and 4 in four of the patients, but all symptoms were manageable.
Overall, the team was delighted to report that in the initial investigation the treatment induced a significant response in 80% of participants and that any adverse events were manageable, allowing this ground-breaking therapy to advance towards the next stage of trials. The team will report further results and updates on this trial at the AACR Virtual Meeting.