Regenerating the heart

Researchers demonstrate regenerative capability of placental Cdx2 cells in mouse model of heart attack.
Researchers from the Icahn School of Medicine at Mount Sinai (NY, USA) have recently demonstrated the regenerative capabilities of the placental derived Cdx2 cells, showing that they are able to regenerate healthy heart cells in an animal model following a heart attack.
“Cdx2 cells have historically been thought to only generate the placenta in early embryonic development, but never before were shown to have the ability to regenerate other organs, which is why this is so exciting. These findings may also pave the way to regenerative therapy of other organs besides the heart,” commented principal investigator Hina Chaudhry.
“They almost seem like a super-charged population of stem cells, in that they can target the site of an injury and travel directly to the injury through the circulatory system and are able to avoid rejection by the host immune system.”
-
How does the liver regenerate?
-
Source of new neurons for the hippocampus
-
Cardiac tissue cultures – out now in 3D!
In previous research the team had found that a mixed population of mouse placental stem cells can repair the hearts of pregnant female mice. After migrating to the damaged region, the placental stem cells were able to reprogram themselves as beating heart cells and helping the repair of an injury that could otherwise lead to heart failure.
The latest study, recently published in Proceedings of the National Academy of Sciences, aimed to determine which type of stem cell could make the heart regenerate. Of the mixed stem cell population, Cdx2 cells were the most prevalent and therefore provided the starting point for their study. They were found to form the highest percentage of placental derived cells assisting the heart, forming around 40% of the cells in question.
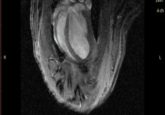
In order to test the regenerative capability of the Cdx2 cells, the researchers induced a heart attack in three groups of male mice. The first group received Cdx2 placental stem cell treatments, the second group received non-Cdx2 expressing placenta cells and the final group received a saline control. Using MRI to analyze mice immediately after, as well as 3 months post heart attack, they found that every mouse in the Cdx2 treatment group had significant improvement and regeneration of healthy tissue in the heart. At 3 months, the cells had migrated to the heart and began to form new blood vessels and cardiomyocytes. All of the mice in both the saline and non-Cdx2 cell group went into heart failure, none of them displaying any evidence of regeneration.
“…No other cell type tested in clinical trials of human heart disease were ever shown to become beating heart cells in petri dishes, but these did and they knew exactly where to go when we injected them into the circulation.”
“These results were very surprising to us, as no other cell type tested in clinical trials of human heart disease were ever shown to become beating heart cells in petri dishes, but these did and they knew exactly where to go when we injected them into the circulation,” commented Sangeetha Vadakke-Madathil, the first author of the study.
The researchers also noted two further properties of the Cdx2 cells: they have all of the proteins of embryonic stem cells as well as additional proteins that give the cells the ability to travel to the site of injury, something that embryonic stem cells lack. The immune system showed no signs of rejection when the cells were administered from the placenta to another animal.
“These properties are critical to the development of a human stem cell treatment strategy, which we have embarked on, as this could be a promising therapy in humans. We have been able to isolate Cdx2 cells from term human placentas also; therefore, we are now hopeful that we can design a better human stem cell treatment for the heart than we have seen in the past,” explained Chaudhry.
“Past strategies tested in humans were not based on stem cell types that were actually shown to form heart cells, and use of embryonic stem cells for this goal is associated with ethics and feasibility concerns. Placentas are routinely discarded around the world and thus almost a limitless source.”