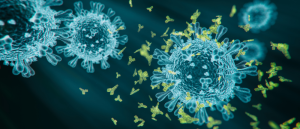
Benefit of breastmilk: COVID-19 antibodies pass from vaccinated mothers to infants

Study detects neutralizing antibodies against SARS-CoV-2 in stool samples of infants breastfed by vaccinated mothers with the potential to provide passive immunity against the virus.
Researchers from the University of Massachusetts (MA, USA) assessed the immune composition in breastmilk from mothers who had received an mRNA-based COVID-19 vaccine and the potential transfer of protective antibodies to breastfeeding infants. The study, led by Vignesh Narayanaswamy, found that milk from immunized mothers neutralized the SARS-CoV-2 spike protein and the immune response was reflected in breastfed infants. The results provide reassurance to breastfeeding mothers and expecting mothers alike.
“This is really important because women want to know whether their babies have these antibodies, and our study shows that antibodies are being transferred via breast milk. Providing this compelling evidence is motivation for women to continue breastfeeding after they receive the vaccine,” Narayanaswamy highlighted.
Thirty lactating women across the United States who were expecting to receive, or recently received, the Pfizer or Moderna mRNA COVID-19 vaccine were enrolled in the study. Breastmilk samples were donated before vaccination, across 2–3 weeks after the first dose and across 3 weeks after the second dose. For comparison, stool samples from breastfed infants were also collected 21 days after the mothers’ second dose. All samples were tested for SARS-CoV-2 receptor-binding domain (RBD)-specific IgA and IgG using enzyme-linked immunosorbent assay (ELISA).
 COVID-19 autoantibodies: could sex influence susceptibility to long COVID-19?
COVID-19 autoantibodies: could sex influence susceptibility to long COVID-19?
Researchers report that COVID-19 can induce self-attacking autoantibodies persisting up to 6 months post-infection and show sex-specific differences in the immune response.
Milk samples from 26 out of 30 mothers donated more than 2 weeks after the second vaccination tested positive for anti-RBD IgG and 14 out of 30 mothers’ milk samples were positive for anti-RBD IgA. Interestingly, antibody levels detected in the milk were not found to be linked to the lactational stage or the child’s age – Narayanaswamy emphasizes that this was an important finding of the study.
The milk samples indeed neutralized the SARS-CoV-2 spike protein and four variant proteins of concern including D614G, Alpha, Beta and Gamma. This immune response was mainly driven by anti-RBD IgG. Similarly, the pattern of immune response to maternal vaccination was mirrored in the breastfed infant stool samples, in which 33% and 30% were positive for anti-RBD IgG and anti-RBD IgA, respectively.
Another fascinating finding from the study revealed that the levels of antibodies found in the infants’ stool correlated with the severity of side effects that the mother experienced post-vaccination. “Women who did feel sick from the vaccine was associated with greater antibodies in the infant stool,” senior author Kathleen Arcaro explained. “So you might have felt badly, but that was a benefit for your infant.”
These results come after a recent case study revealed that a mother, vaccinated with her second dose 3 days prior to the healthy delivery of her child, produced vaccine-generated antibodies in the umbilical cord. This builds a strong case to support the vaccination of pregnant mothers and the theory that a degree of immunity can be passed from a mother to her child through several routes.
The compelling results may be a motivation for women to continue breastfeeding after receiving a COVID-19 vaccine, particularly since lactating and pregnant women are being urged to be vaccinated but were not included in the vaccine trials. Arcaro reassures that the findings demonstrate that “even if you had COVID, there is a benefit for women to get the vaccine.”