How is cancer immunology being utilized in the fight against cancer?
Cancer immunology refers to the immune system’s role in the progression and development of cancer. As with all disease, our bodies have certain immune defenses intended to protect us from tumor development. However, tumor cells have developed ways to evade immune surveillance, and can even create immunosuppressive tumor microenvironments to develop without interference from the immune system.
For the last few decades, cancer immunology research has focused on taking what we know about our immune response to cancer and cancer’s defense against this to develop new treatments for cancer patients, known as immunotherapy.
Cancer immunology: what is immunotherapy?
In general, cancer immunotherapy involves using natural or synthetic substances to restore or enhance the patient’s immune system, allowing the body to ‘naturally’ fight off cancer. Many patients view this as preferable over traditional chemotherapeutic methods, as it’s utilizing the body’s own resources rather than using toxic chemicals to destroy the tumors.
The first US FDA approved cancer treatment utilizing cancer immunology was the Bacillus Calmette–Guérin (BCG) vaccine, which was approved for bladder cancer treatment back in 1990. Since then, there have been huge developments in the field of cancer immunotherapy and, as of December 2019, the FDA has approved immunotherapy treatments for nearly 20 different cancer types.
Immunotherapies have already seen huge successes in several cancer types, such as in metastatic melanoma where combination immunotherapy drugs are the only successful treatment option. Researchers working in the field believe that immunotherapy has the potential to provide effective treatment for every type of cancer.
Immunotherapy types
Immunotherapies currently in use for the treatment of cancer can be broken down into five main types: adoptive cell therapy, targeted antibodies, cancer vaccines, immunomodulators and oncolytic virus therapy.
Adoptive cell therapy
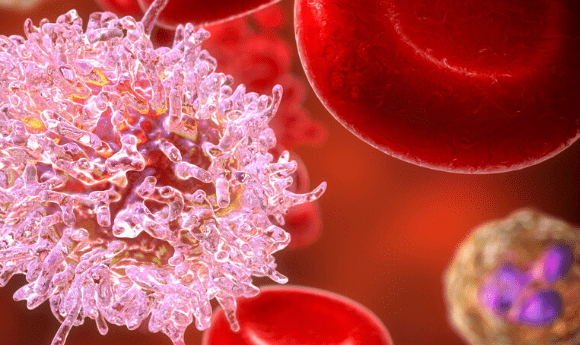
Adoptive cell therapy involves taking advantage of the body’s natural defenses by using immune cells (either isolated from the body or genetically engineered in the laboratory) to destroy cancerous cells.
The form of this treatment that has experienced the highest level of clinical success is CAR-T Cell therapy. This involves isolating or generating T cells and equipping them with a synthetic chimeric antigen receptor (CAR). These antibodies are then transfused back into the body where they bind with the proteins on the cancer cells surface and destroy them.
Some other applications of adoptive cell therapies, which all follow the same general principle as CAR-T, are; tumor-infiltrating lymphocyte therapy, where naturally occurring T cells that have already entered the patient’s tumor are isolated, activated and expanded in the lab before being reinfused back into the patient; and engineered t cell receptor therapy, where a patients T cells are harvested and armed with new t cell receptors that target specific cancer antigens.
There are only two types of adoptive cell therapy currently approved by the FDA, and both are a form of CAR-T therapy designed to treat leukemia and lymphoma. There are currently many other adoptive cell therapies under evaluation in clinical trials in the US, such as mesothelin‑directed CAR T therapy to treat a range of cancers including malignant mesothelioma and breast cancer. Researchers are also working on utilizing new cell editing techniques, such as CRISPR, to heighten the effectiveness of current and potential therapies.
Targeted antibodies
Another type of immunotherapy is engineering antibodies that are able to target cancer antigens. This is considered a form of passive immunotherapy, as it involves targeting tumor cells directly rather than the immune cells.
Traditionally, monoclonal antibody treatment involved treating patients with antibodies that would bind to cancer cells and prevent them from growing, whilst also sending signals to other immune cells to stimulate the destruction of the tumor cells. The first targeted antibody cancer treatment was approved by the FDA in 1997 for Non-Hodgkin’s lymphoma, though its approved uses have since been expanded, and since then 18 more therapies of this kind have been approved, including necitumumab, a monocolonal antibody used in conjunction with chemotherapy drugs to treat previously untreatable metastatic squamous non small cell lung cancer.
In recent years, researchers have refined this therapy type to produce antibody drug conjugates. This involves treating patients with antibodies loaded with anti-cancer drugs, which are released into the body upon binding with the cancer cell and act to directly kill the cancer cell. This has been successful so far, with 9 antibody-drug conjugates currently earning FDA approval.
Cancer vaccines
Cancer vaccines generally utilize the same principles as vaccines of viral or bacterial infections, with the main difference being that, unlike bacteria and viruses, cancer cells are not ‘foreign’ and can quite closely resemble healthy cells. Therefore, in order to develop vaccines to prevent or fight cancer, more sophisticated techniques must be used.
There have been a reasonably high number of successes in developing preventative vaccines for cancers where development is stimulated by viral infection. For example, it has been discovered that HPV infection can result in the development of cervical or head and neck cancer and, in theory, developing a vaccine against HPV should help protect individuals both from the viral infection and the consequential cancer development.
There are currently four preventative cancer vaccines approved by the FDA, including three to prevent HPV infection and one to protect against hepatitis B infection, which researchers have shown to be responsible for the development of certain liver cancers.
Less success has been found in developing therapeutic cancer vaccines to target specific tumor antigens. This is due to each individual’s tumor being unique with slightly different antigens on each tumor cell. However, there have been some successes, and two therapeutic cancer vaccines are approved by the FDA: BCG which stimulates immune system to fight early-stage bladder cancer and Sipuleucel-T, which targets proteins on prostate cancer cells.
Immunomodulators
Immunomodulators are molecules that regulate the activity of the immune system. Immunotherapies involving immunomodulators utilize the molecules to enhance the body’s natural immune defenses to destroy cancer cells. This field of immunotherapy is the area that has seen the highest level of success over recent years.
Immunomodulators can be divided into four broad types: Cytokines, messenger molecules that regulate immune cell maturation, growth and responsiveness; agonists, molecules that activate pathways and promote adaptive immune responses; adjuvants, molecules that activate innate immune pathways and enhance general immune responses; and checkpoint Inhibitors, which block immune checkpoints to enhance immune responses against cancer cells.
There are currently 14 different immunomodulators approved by the FDA for the treatment of a range of different cancer. Immune checkpoint inhibitors have experienced the highest success rates, with seven of these approved therapies representing immune checkpoint inhibitors alone. The first was approved only in 2015, demonstrating how fast the field is developing. Furthermore, several single immune checkpoint inhibitors, including pembrolizumab and nivolumab, have demonstrated success in treating a wide range of different cancer types, increasing the overall value of the drugs.
Oncolytic virus therapy
For oncolytic virus therapy, cancer cells are infected with certain viruses, known as oncolytic viruses, which then attack and destroy the tumor. Cancer cells themselves have impaired antiviral defenses, leaving them vulnerable to infection. Furthermore, once the virus infects the tumor cell, the cell explodes and releases the cancer antigens, which can then go on to stimulate further immune responses to destroy the remaining tumor cells.
Whilst there is currently only one form of the therapy with FDA approval, a modified herpes simplex virus to treat certain melanoma patients, it is believed that this treatment has the potential to be very effective. Current clinical trials in the US are evaluating the use of a range of other viruses including measles, picornavirus and adenovirus to treat a range of different cancers in this way.
How effective is immunotherapy?
Whilst several trials have demonstrated very high effectiveness in the treatment of different cancer types, the level of effectiveness for different immunotherapies are extremely variable. Factors affecting the effectiveness include the type and length of treatment; biological characteristics of the patient and the cancer, and lifestyle factors such as diet and exercise.
To improve the effectiveness of immunotherapy, further study into cancer immunology is required, there have been increased efforts to develop predictive biomarkers, which would allow researchers to determine the most effective therapy before administration. Recently, there have considerable advances in developing immunotherapy predictors, including research that demonstrates potential applications for artificial intelligence, as well as the discovery of the role the gut microbiota could play in predicting immunotherapy response.
Developments in the field over the past 30 years has allowed immunotherapy to establish itself as a vital pillar of cancer treatment. Amongst many oncologists, there is even a feeling that immunotherapy may render chemotherapy obsolete in the future, though others believe that a combination of the two therapies will become the new ‘gold standard’ treatment.
Regardless of what the future holds in terms of the position of immunotherapy in cancer treatment, we can be sure that there is still a lot of research needed until the true potential of cancer immunology is determined.