Demystifying the immune system’s function as a spam filter
 How does our innate immune system recognize and exclude potential threats so efficiently? Javier Irazoqui, an Associate Professor of Microbiology and Physical Systems at the University of Massachusetts Amherst (MA, USA), and his lab group study the mechanisms of host-microbe interactions in both healthy and diseased states, hoping to answer that very question.
How does our innate immune system recognize and exclude potential threats so efficiently? Javier Irazoqui, an Associate Professor of Microbiology and Physical Systems at the University of Massachusetts Amherst (MA, USA), and his lab group study the mechanisms of host-microbe interactions in both healthy and diseased states, hoping to answer that very question.
Here, Irazoqui discusses the challenges of studying these interactions, the brain-gut-microbiota axis and the techniques used to demystify this sophisticated system.
Could you explain the focus of your research?
Fundamentally, the research in my lab focuses on how our immune system manages to function as an email spam filter – allowing the microbes that keep us healthy to thrive, while excluding those that make us sick. Somehow, within minutes of contact, our bodies discriminate and make the decision whether to let a new microbe through or block it. This is the work of the ‘innate’ immune system. But how does the innate immune system do that so quickly and so well? Despite being bombarded with potentially harmful bacteria, viruses and fungi, most of us don’t get sick all the time so we know it works remarkably well. But what goes wrong when a microbe does get through and makes us sick? How can we learn from that to improve upon Nature, to develop new therapies for infections? The other side of the coin is when the body goes haywire and sees a threat where there is none, like allergies, gut inflammation, skin inflammation, or brain inflammation. What happens in those cases? Why does the innate immune system overreact? How can we dampen it to treat diseases? These are the questions we seek answers for.
What sort of host-microbe interactions do you study?
We take a pretty holistic approach to what we call the host. In our studies, we like to use the entire organism and study processes in vivo. This means embracing pretty sophisticated and complex questions about how the entire organism – its metabolism, growth, reproduction, overall health, and at the genetic and molecular levels – adapts to infections to fight disease. We use models to learn about human health.
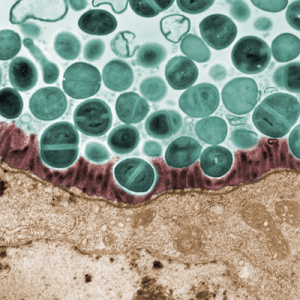
Models (or model organisms, in our case) are animals that share many of the key features of human immune systems, so the hope is that by learning about one organism we learn more about human health and disease. In our lab, our main model organism is the animal Caenorhabditis elegans (C. elegans). This is a tiny roundworm (think smaller than a grain of rice, not the kind you find in your garden and you use as bait!). For decades, C. elegans has helped scientists around the world learn about neuroscience, development, reproduction and genetics of humans. More recently, we have been using it as a model to understand fundamental aspects of host defense against infection, which is an extreme case of host-microbe interactions. Other examples of host-microbe interactions may include cases where the microbe gets eliminated upon the first encounter (as most do), or more interestingly, to me at least, when the microbes and the host establish a mutually beneficial and stable relationship – called symbiosis.
Here in my lab, we focus on host-pathogen interactions (infections) with pathogens like Staphylococcus and Pseudomonas, which cause a lot of harm worldwide. We also study what is different in bugs that reside peacefully in the host gut and help the host stay healthy.
What are the challenges of studying these interactions?
 What makes these interactions fascinating to me is that here you have two living organisms (the microbe and the host) that are ‘talking’ to each other through molecules. What are these molecules? How are they produced? What effects do they have? How does this conversation change over time? These are major questions that the field is addressing. The challenge is technological, being able to ‘see’ the ‘right’ molecules in the right places at the right times, and conceptual, what defines a molecule as ‘right’? Of course, when we’re not talking about a single microbe but whole communities, things get way more complicated and harder to understand, much like at family gatherings! But if we hope to understand human biology, we need to explore this.
What makes these interactions fascinating to me is that here you have two living organisms (the microbe and the host) that are ‘talking’ to each other through molecules. What are these molecules? How are they produced? What effects do they have? How does this conversation change over time? These are major questions that the field is addressing. The challenge is technological, being able to ‘see’ the ‘right’ molecules in the right places at the right times, and conceptual, what defines a molecule as ‘right’? Of course, when we’re not talking about a single microbe but whole communities, things get way more complicated and harder to understand, much like at family gatherings! But if we hope to understand human biology, we need to explore this.
What is the brain-gut-microbiota axis?
We use the term ‘brain-gut-microbiota axis’ to describe an important system in our bodies that influences every aspect of our lives, from our health or disease to our behavior and emotions. The system consists of three parts.
The microbiota is the community of microbes that lives in our guts. This is the main place where we get colonized by thousands of different species of bacteria, and also viruses and fungi, which are kind of the ‘dark matter’ of the microbiota.
In the brain-gut-microbiota axis, goings-on in the brain influence the way the gut works, including the immune system, which changes the membership (or composition) and behavior of the microbiota. This works both ways as the microbiota, in its behavior and membership, influences the immune system, which in turn talks to the brain and influences our moods and behavior. We also know of some ways that the microbiota talks directly to the brain.
This axis is important not only for our healthy living but also plays a large role in chronic inflammation (think inflammatory bowel disease or arthritis) and in obesity, diabetes, and even neurodegenerative diseases like Parkinson’s and Alzheimer’s.
Could you tell me more about your research on the brain-gut-microbiota axis and the techniques you use to investigate this?
There are many more unknowns about this axis than knowns, frankly. We know some of its roles, but probably not all – and even in the cases that we are aware of, we still don’t understand exactly what happens and in what order, in health or in disease. We’re working on it, but it takes time to make progress. What we have discovered is that the nervous system (in C. elegans, at least) directly talks to the intestine through the neurotransmitter acetylcholine. Acetylcholine is what makes muscles contract; it also plays important roles in the nervous system and in the immune system. What we discovered is that acetylcholine in the nerves goes to the gut, and there it changes gene expression. The genes that are turned on are important antimicrobials and cell repair genes. The whole system, from acetylcholine to the gut and genes, is turned on during infection. What we don’t know is how the brain knows that the organism is infected. How does it release acetylcholine? What kinds of roles do the antimicrobial and repair genes actually play in infection and inflammation? How can we hack the system to our benefit, to help clear infection faster and better, or diminish inflammation with fewer side effects?
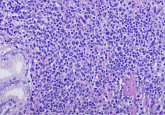
In my lab, the research is driven by our hunger to answer these questions and for that, we use a broad array of techniques. We don’t shy away from adopting new techniques if they help us get an answer better or faster. We are using optical techniques like light and electron microscopy to ‘see’ the infection and the immune system in action in live C. elegans and in mammalian cells. We use genetics and genome editing (CRISPR) to specifically pinpoint the contribution of each interesting gene to the overall health or disease of the organism (host and microbe!). We use protein and nucleic acid biochemistry to understand how the genes actually produce the effects that we observe in vivo. Finally, we use metabolomics approaches to get a better picture of what the ‘right’ molecules are that drive the conversation between host and microbe.
What is next for your research?
It’s hard to tell because so much of it is dynamic and defined by the results that we are getting. I can envision two major directions though. One is to really define the molecules that the microbe produces that ‘tickle’ the brain to release acetylcholine. We are using microbial genetics and metabolomics to get at that. Another is to understand, at a molecular level, the sequence of events that link that first encounter to the turning on of genes that enhance host health. We are using genomics and genetics and cell biology to study this, and our main interest is about the strongest ‘switches’ that turn on and off the immune response. We hope that answering these questions will give us clues to how to manipulate the brain-gut-microbiota axis to improve human health.
What does Hispanic Heritage Month mean to you?
To me, Hispanic Heritage is a complicated concept. Sometimes we forget the worldwide impact of the Spanish Empire in the 15th and 16th centuries, which still reverberates today. On top of a history of colonialism and oppression, there is a history of cultural unity and diversity that enriches our lives even today. From Tierra del Fuego to the Northernmost reaches of the Spanish Empire in what today is the USA, we are at once united by a common history and influenced by the broad diversity of cultures within what is the Hispanic Americas. The Spanish language is a powerful force that underlies our cultural heritage and unites us in the English-speaking world. To me, Hispanic Heritage Month is a time of reflection and learning, about our history, our cultural inheritance, and our responsibility. It is also a time of joyful celebration of our diversity and traditions.
Are there any up-and-coming Hispanic scientists or organizations that you’d like to shout out?
There are so many. I don’t want to pick favorites. I have been impressed by the work of countless individuals that overcome sometimes crippling adversity to become impressive scientists and to serve the Hispanic and broader scientific community. I am passionate about mentoring and about science communication and have been very impressed by organizations like SACNAS, ABRCMS, and Ciencia Puerto Rico, which effect real-world change in diversity and representation in science.