Managing mucin secretion
The proteins responsible for the control of mucin secretions, a key component of protective mucus, have been established in two recent papers.
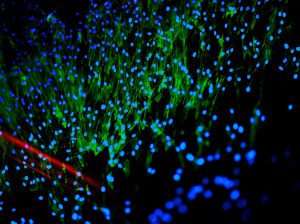
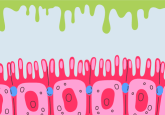
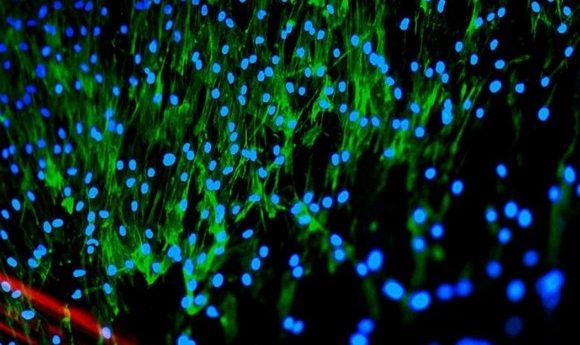
Mucins, the vital proteins that compose the protective mucosal lining of the airways and intestines, have previously been poorly understood with regard to their regulation and secretion. New research from a collaboration of researchers from the Centre for Genomic Regulation (CRG; Barcelona, Spain) and the Pompeu Fabra University (Barcelona, Spain), however, has shed light on the regulation of mucin release from specialized goblet cells, finding three proteins that played key roles in the pathway.
While it has been established that the control of mucin secretion is largely influenced by calcium, the actual pathways and processes through which this control is enforced are poorly understood. Gerard Cantero-Recasens and Vivek Malhotra (CRG), the leaders of the collaboration, set out to discover mechanics and molecular participants involved in these pathways.
Firstly, a genome-wide screen was deployed to identify any proteins involved in mucin secretion in colon cancer cells. This approach initially identified 25 proteins. Using various biochemical assays in a selection of different cell lines, the research team were able to narrow down the search to three key players in the regulation of mucin secretion.
“This is an exciting finding because it means targeting the molecules involved in mucin secretion process can be used to treat airway diseases such as asthma or chronic obstructive pulmonary disease, as well as the colon associated pathologies.”
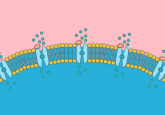
The first two proteins indicated were the surface proteins known as Na+/Ca2+ exchanger 2 (NCX2) and transient receptor potential cation channel subfamily M member 4 (TRPM4), which collaborate to control calcium transport into the cell and therefore the calcium-mediated secretion of mucins. The research team then blocked the activity of NCX2 and TRPM4 in a normal bronchial epithelial cell line from patients with cystic fibrosis, which resulted in a reduction in the secretion of the mucin MUC5AC.
A second paper documents the third protein KCNIP3, which acts as an intracellular control of mucin secretion. The calcium-binding protein is usually bound to mucin secretory granules, acting as an inhibitor to exocytosis. When the intracellular levels of calcium fluctuate, KCNIP3 dissociates from the vesicles and they are free to fuse with the cellular membrane, secreting their mucin content into the mucus.
“We were surprised by this finding – we didn’t expect that cells use different sources of calcium – from internal and external sources – to control mucin secretion. We also didn’t expect to find that the KChIP3 sensor controlling baseline (basal) mucin secretion does it by acting like a ‘brake’ to prevent mucin release,” commented Cantero-Recasens.
The study also found that these cellular processes were the same for the airways and in the intestinal tract. “This is an exciting finding because it means targeting the molecules involved in mucin secretion process can be used to treat airway diseases such as asthma or chronic obstructive pulmonary disease, as well as the colon associated pathologies,” explained Cantero-Recasens
Naturally, the next step for this research is to examine the genes encoding these proteins to see if they have common alterations and to design chemicals that can target the proteins to induce specific functions. If successful these studies could yield novel approaches for the treatment and diagnosis of asthma, chronic obstructive pulmonary disease, irritable bowel disease and colorectal cancers.