Schizophrenia’s effect on synaptic function

Current treatments for schizophrenia come with debilitating side effects—but developing better options is difficult when so little is known about the etiology of this neuropsychiatric disorder. New stem cell models may offer the solution.

Schizophrenia is a devastating neurodevelopmental disorder that affects approximately 1% of the population. Its hallmark symptoms—hallucinations, disordered thinking, delusions, and cognitive impairment—take their toll on individuals with the disease. Yet, antipsychotic medications often don’t treat all of the symptoms. or they come with terrible side effects that get in the way of treatment compliance. Changhui Pak, a neuroscientist at Stanford University, believes that designing better targeted treatments depends upon a clearer understanding of what’s happening in the brain at the molecular level.
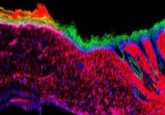
“We decided to focus on the synapse, the fundamental unit of neural communication. We wanted to understand how synaptic function might be affected in individuals with schizophrenia,” she explained. Previous work suggested that a mutation in NRXN1, a gene that increases the risk for developing schizophrenia ten-fold, might affect neural signaling. But the researchers were not sure how that occurred.
To find out, Pak and colleagues created induced pluripotent stem cell (iPSC) models using neurons taken from patients with schizophrenia with NRXN1 deletions and compared them to iPSC models taken from age- and gender-matched healthy controls. They grew these iPSC-generated neurons in the presence of mouse astrocytes to help support them. The two model neurons looked very similar morphologically, but when the researchers took a closer look at synaptic function, they found important differences, which Pak presented at Neuroscience 2017, the annual meeting of the Society for Neuroscience.
“We saw a very specific reduction in the synaptic activity of the schizophrenia neurons, as well as a significant reduction in neurotransmitter release,” she said. “But even more surprisingly, we found that the astrocytes grown with the schizophrenia neurons showed very distinct changes in gene expression patterns, suggesting that there is some unknown mechanism that impairs proper signaling or cell crosstalk between the neurons and the astrocytes.”
Pak and colleagues plan to further investigate that mechanism. In the meantime, she believes this work will help further elucidate the neural pathogenesis involved with schizophrenia, as well as a host of other neuropsychiatric disorders with a genetic basis.
“This approach provides a new platform to probe the origins of other neurodevelopmental and neurodegenerative disorders, which are also thought to affect neural signaling,” she said.