Engineered spinal cord implants provide hope for those with traumatic injury
Using fatty tissue, called adipose tissue, researchers have created an implant that restored movement in both acute and chronic models of paralysis.
For many, a severed spinal cord means a complete lifestyle change and can cause both physical and mental challenges. A team of researchers, led by Tal Divir from the Sagol Center for Regenerative Biotechnology (Tel Aviv, Israel), hope to solve paralysis caused by traumatic injury available to patients soon. Results from a recent study published in Advanced Science have shown the success of an implant that mimics early-stage development of the spinal cord, and the next step is a phase-1 clinical trial.
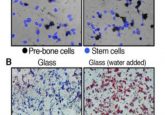
When looking at adipose tissue on a micro-scale, you could say it consists of two components – cells and a gel-like substance called the extracellular matrix (ECM). In this study, researchers took a biopsy of adipose tissue and separated these two components. The team then used the ECM from the adipose biopsy to create a hydrogel that acts as a supporting scaffold for the spinal cord implant. In this scaffolding role, the hydrogel can mimic the microenvironment of embryonic development while avoiding rejection or an immune response caused by foreign bodies.
In addition to lipid cells, adipose tissue also has a high concentration of stem cells, making it the focus of many regenerative medicine researchers. Dvir and his team harvested these stem cells and engineered them to resemble embryonic cells. By maturing these cells carefully within the microenvironment of the hydrogel and using previously established techniques, Divir was able to mimic the spinal cord differentiation seen in embryonic development.
 Hold the antibiotics: next-generation hydrogels have arrived
Hold the antibiotics: next-generation hydrogels have arrived
Scientists have created a new class of non-antibiotic hydrogel capable of fighting multidrug-resistance bacterial infections by enhancing the skin’s natural immune defense.
In porcine models, the team used these spinal cord implants to treat both long-term and short-term paralysis cases. The results are extremely encouraging for a large-scale in vivo study, with 100% of short-term paralysis, and as high as 80% of those with long-term paralysis, regaining their ability to walk.
“This is the first instance in the world in which implanted engineered human tissues have generated recovery in an animal model for long-term chronic paralysis – which is the most relevant model for paralysis treatments in humans.” Explained Divir. “Our goal is to produce personalized spinal cord implants for every paralyzed person, enabling regeneration of the damaged tissue with no risk of rejection.”
The next steps following such promising results are well underway with the development of a spin-out company based upon the technology and first phase clinical trials on the horizon in coming years. Hopefully, this study can provide hope to many that developments such as these spinal cord implants may be just around the corner.