Hold the antibiotics: next-generation hydrogels have arrived

Scientists in Sweden have created a new class of non-antibiotic hydrogel capable of fighting multidrug-resistant (MDR) bacterial infections by enhancing the skin’s natural immune defense.
A recent study led by co-first authors Yamiao Fan, from the KTH Royal Institute of Technology (KTH RIT; Stockholm, Sweden), and Soumitra Mohanty (Karolinska Institutet and Karolinska University Hospital both Stockholm, Sweden), reveals a new treatment in the fight against antibiotic resistance. The team developed a dendritic macromolecule-based polymer hydrogel and evaluated the material for cytotoxicity and antibacterial capabilities. The study demonstrates a new class of cationic dendritic hydrogels capable of eliminating bacterial skin infections caused by MDR bacteria.
Antibiotic-resistant bacterial infections are a global threat to which biomaterials such as hydrogels provide an appealing solution, due to their antibiotic-like properties – without the antibiotics. In this study, the authors demonstrate the benefits of a new type of hydrogel modeled on hyperbranched dendritic polymers, which are thought to interact with bacteria through numerous cationic, charged contact points disrupting the bacteria.
Although the exact mechanism by which the hydrogel is successful is yet to be elucidated, one thing is for certain, “their well-designed, branched structure and scalability makes them ideal scaffolds for biomedical applications,” explained senior author Michael Malkoch (KTH RIT).
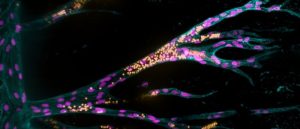 The first functionally vascularized synthetic hydrogel
The first functionally vascularized synthetic hydrogel
In a world-first, researchers have developed a synthetic hydrogel scaffold that can be functionally vascularized.
The hydrogels were tested against clinically significant infectious Gram-positive and Gram-negative bacteria, including the pathogens Escherichia coli, Staphylococcus aureus (S. aureus) and Pseudomonas aeruginosa. The hydrogels exhibited 100% killing efficacy towards all three pathogens at bacterial concentrations 105–108 CFU mL-1. The study also demonstrated that the hydrogel is more effective at killing methicillin-resistant S. aureus (MRSA) than the hydrogels available in current wound dressings.
“Dendritic hydrogels are excellent for wound dressing materials because of their soft, adhesive and pliable tactile properties, which provide ideal contact on the skin and maintain the moist environment beneficial for optimal wound healing,” Malkoch illuminated.
Not only do the new hydrogels kill drug-resistant strains isolated from wounds; they also promote the expression of endogenous antibiotics, which were shown to promote host-mediated bacterial killing in human keratinocytes. “Contrary to traditional antibiotics, where bacteria may develop resistance quickly, resistance towards antimicrobial peptides, is very rarely seen,” co-author Annelie Brauner described.
Ultimately the hydrogels have excellent biocompatibility, degradability, anti-inflammatory properties as well as the ability to promote host-mediated bacterial killing. “The gel is an outstanding contribution in the fight against multidrug-resistant bacteria – especially in current times, when we are running out of available antibiotics,” Brauner expressed hopefully.