Looking at the big picture in childhood cancers
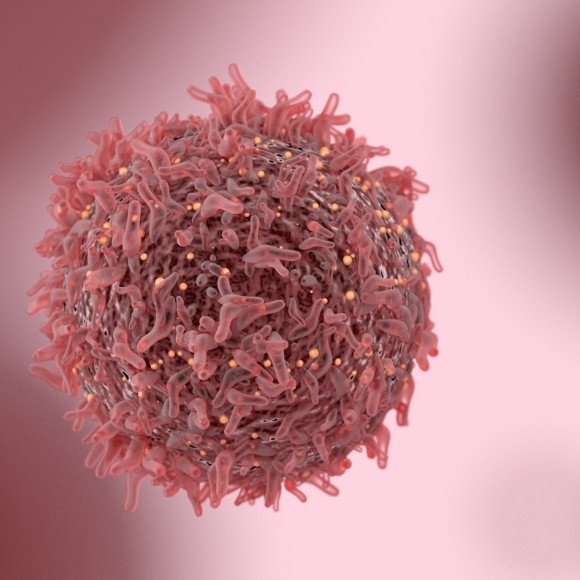
Everybody knows images are worth a thousand words, but could their value be even higher when it comes to pediatric brain cancers?
Peter de Blank graduated from the University of California, San Francisco School of Medicine (CA, USA) with a concentration in medical education. He completed his residency in pediatrics, and fellowships in pediatric hematology & oncology and pediatric neuro-oncology at the Children’s Hospital of Philadelphia (PA, USA). He completed a Master’s of Science in clinical epidemiology and biostatistics at the University of Pennsylvania (PA, USA) during his fellowship training.
After his training, he became a faculty member at University Hospitals Rainbow Babies & Children’s Hospital in Cleveland (OH, USA) in 2012. In 2017, de Blank joined the faculty at Cincinnati Children’s Hospital Medical Center (OH, USA) as a member of the pediatric neuro-oncology program. de Blank’s clinical and research interests include children with CNS tumors, neurofibromatosis type 1 (NF1), and NF1-related tumors.
Based on his progress to date, de Blank was awarded a new grant from the St. Baldrick’s Foundation in 2017. This was in order to fund an additional year of the St. Baldrick’s Scholar award to support his research focused on investigating a new radiographic tool to diagnose brain tumors prior to surgery and define the extent of the tumor’s invasion. This tool aims to improve outcomes by identifying children at risk for tumor recurrence and poor outcomes.

What is your scientific background, what do you do now and how did you get there?
I completed medical school at the University of California, San Francisco with an emphasis in medical education. I then completed my residency in pediatrics and a fellowship in pediatric hematology and oncology at the Children’s Hospital of Philadelphia. During my training in oncology, I completed a Master’s of Science in clinical epidemiology and biostatistics from the University of Pennsylvania.
After my fellowship, I completed an additional fellowship in pediatric neuro-oncology from the Children’s Hospital of Philadelphia. During that time, I studied advanced MRI techniques including diffusion tensor imaging (DTI). After my training, I became faculty at Rainbow Babies & Children’s Hospital and Case Western Reserve University School of Medicine (OH, USA) as a pediatric neuro-oncologist. There, I continued my research in quantitative MR techniques including magnetic resonance fingerprinting and synthetic MR techniques through grants from the St. Baldrick’s Foundation and the Neurofibromatosis Therapeutic Acceleration Program at Johns Hopkins University (MD, USA).
In 2017, I took a position at Cincinnati Children’s Hospital Medical Center as an associate professor and a pediatric neuro-oncologist.
Can you tell us about your research?
My research is in non-invasive, quantitative MR methods to measure tissue characteristics in children with brain tumors. We hope that these imaging techniques will go beyond the pretty picture and tell us important aspects about pediatric tumors, including diagnosis, tumor grade, and functional outcomes. I also am particularly interested in low-grade gliomas of childhood, which are frequent in children with NF1.
What have you discovered?
We have shown that DTI can be useful in measuring vision loss in children with low-grade gliomas in the optic pathway. DTI uses the natural diffusion of water in the brain to locate white matter tracts connecting regions of the brain, such as the visual pathway. By measuring the diffusion that leaks out across membranes, we can quantify the integrity of these connections.
In our research, we’ve shown that integrity of white matter tracts in the optic radiations correlates with visual acuity in children with optic pathway gliomas and may predict future vision loss. Since preserving vision is one of the most important goals of therapy for this tumor, measuring vision accurately is vitally important, but very young children often have difficulty with traditional vision tests because of decreased attention.
We hope that DTI can combine with traditional vision tests and other experimental techniques that measure damage (such as optical coherence tomography) to more accurately measure visual acuity and potentially predict vision loss to help identify young children who might benefit from therapy for this tumor.
I also study quantitative relaxometry methods such as magnetic resonance fingerprinting (MRF). MRF is a technique that produces rapid, simultaneous quantitation of tissue parameters such as T1 and T2 relaxation time. To do this, MRF uses pseudo-randomized acquisition parameters to generate a multi-parametric data signal that is then matched in each voxel to a dictionary of all possible calculated signal evolutions in order to produce a parameter map. This fast imaging technique has continued to accelerate and now offers whole-brain imaging with clinical resolution in less than 5 minutes with remarkable parameter accuracy and efficiency.
In our research, we’ve shown that T1 and T2 values derived from MRF can help distinguish tumor tissue from healthy brain tissue, as well as high-grade from low-grade tumors in children and young adults with brain tumors. We hope that this technique will help us identify tumor type and grade prior to surgery and may help measure occult disease or response to therapy without needing a biopsy.
The pediatric population presents specific challenges in research. How is this kind of imaging helping to overcome these?
My mentors used to say that every biopsy was a failed imaging experiment. MRI scans should give us more than just beautiful images, they should help us know what type of tumor we see, where it may be hiding, how it is responding to therapy, and how it is affecting a child’s function (such as vision, strength and cognition). Quantitative MR methods have the potential to tell us much more about the tissue they depict, and for kids this could mean fewer trips to the operating room, more certainty about therapeutic responses, and hopefully more cures.
At the same time, these scans are getting both more accurate and faster. For an adult, a faster scan might be more convenient, and for a radiologist it may mean scanning more patients. But for a child, a faster scan can mean less sedation, which means less risk, less time in the hospital and more time enjoying life.
What techniques and technologies do you foresee us using in the future to improve our understanding and treatment of pediatric tumors?
I think we are on the cusp of using advanced MR imaging techniques a lot more frequently. These methods are non-invasive, don’t use ionizing radiation and have the potential to tell us a lot about the diseases and pathologies we treat. As these techniques get better and faster, I think they will supplement or replace many of our traditional imaging sequences.
Soon, I hope we will get to a point where the medical images we take are worth more than a thousand words—they will help us better understand what we are fighting, measure more accurately whether our treatments are working and understand the functional consequences of pediatric brain tumors and their therapies.