Q&A: 3D cell cultures, from development to drug discovery
Kalpana Barnes (Sartorius, London, UK), Robert Vries (Hubrecht Organoid Technology, Utrecht, The Netherlands) and Marta Shahbazi (MRC Laboratory of Molecular Biology, Cambridge, UK) answer your questions following on from the successful panel discussion “3D cell cultures, from development to drug discovery.” Don’t worry if you missed it, you can catch up on demand now & make sure you check out the rest of our spotlight on 3D cell culture here.
Which types of scaffold do you think are best for the purposes of drug discovery?
Kalpana: Scaffolds that are relatively easy to prepare and handle, compatible with automation and don’t interfere with your choice of analytical technique would all be considerations. A good supply chain with associated product quality control would also be desirable. Synthetic scaffolds that offer more precise control of constituents may also be beneficial and preferred over naturally derived scaffolds.
How do we maintain the vasculature in the spheroids or organoids?
Kalpana: There are many advantages to using either spheroid or organoid cultures that we’ve discussed today. However, one disadvantage is that neither incorporate a vasculature so this a driver for next-generation 3D culture models.
How is it possible to avoid necrosis when the spheroids are developed over 400 microns?
Kalpana: Mass transport limitations mean that spheroids of 400 microns or larger in diameter will display gradients to oxygen, nutrients and metabolic waste products. These spheroids will exhibit a common layered structure consisting of a necrotic core, surrounded by a layer of quiescent cells and proliferating cells at the periphery. Creating spheroids of less than 200 microns will avoid the formation of necrotic cores.
Do you use culture media specifically developed for 3D or do you use standard (or non-standard) 2D culture media?
Kalpana: When using cancer cell lines traditionally grown in 2D and creating 3D spheroids using either scaffold-free or scaffold-based techniques, we are using the recommended media for 2D culture. When culturing 3D organoids, we are using specialized media.
Marta: This depends quite a lot on the type of 3D culture. Spheroids, in general, have less strict requirements in terms of media composition. For example, spheroids of mouse embryonic stem cells or human embryonic stem cells can be formed with a simple basal media. However, organoid cultures require more complex 3D formulations that were empirically developed. Each organoid type has slightly different media requirements.
How can a “single organ” organoid replace animal trials? Or are you planning to connect various organoids, as is being done in organ-on-the-chip devices?
Marta: This is an excellent question. All models have positive and negative aspects, and we need to choose the appropriate model to address our experimental question. I don’t think organoids will completely replace animal trials, at least not at the moment. While they are ideally suited to perform drug screening, they cannot be used to assess drug toxicity or side effects. For diseases that involve multiple organs and their crosstalk, organoids would not be very helpful.
Rob: Animal experiments are aimed at studying biology and, in drug development, at testing efficacy and safety in a physiological system. The main issue with the relevance of data from animal studies for humans is that it most often doesn’t reflect results in humans. For this reason, scientists try to develop human models.
With the recent advances in iPSC and adult stem cell-derived organoids we have made a major step in the development of human/patient-relevant models. Therefore, we are able to answer many more of our biological, efficacy or safety questions by using a human relevant model system instead of an animal study. This reduces the use of animals and provides better answers. We will need additional developments to completely replace animals, but it is now coming close.
Human cells such as organoids can be grown in many different systems from simple plastic (multi) well plates to complex microfluidic systems set up on ‘chips’ often referred to as Organ on a Chip. As above the aim of the model is to represent a human. The choice of system depends on the question that needs to be answered. For example, for testing the viability of cells in response to drugs it is preferable to study only the tumor organoid, whereas to study the interaction of endothelium with a tumor the combination is required. This is important because the combination of organs on a chip in itself is not relevant. It is only useful when we are studying the interaction between the organs AND the organ on a chip model mimics the interaction in a physiologically relevant way.
It needs to be considered when developing combination models of organs on a chip, that the connection of organs in a human body is the practical result of evolution: a liver is connected to an intestine by blood vessels etc., to transfer material or communicate. In a laboratory, we have pipettes to transfer molecules and we can simply grow liver organoids and transfer their molecular communication and material or drug metabolites by pipetting to an intestinal organoid, no need to recreate a blood vessel.
 Sylvia Boj on gene editing in organoids and their use in drug discovery
Sylvia Boj on gene editing in organoids and their use in drug discovery
In this interview we catch up with Sylvia Boj, who takes us through a recent paper that used patient-derived organoids as a test case for a new CRISPR technique and talks about the impact this technology could have in the development of organoids for regenerative medicine.
Cancer organoid culture will select for a subpopulation of the tumor in vivo. Can someone please comment on this?
Rob: Data on HUB Organoids (e.g. van de Wetering et al. Cell 2015) shows that a heterogeneous population of cancer cells obtained through resection or biopsy maintains its genetic diversity in culture after long-term passaging. This indicates that this organoid culture method mimics the in vivo conditions such that no in vitro selective pressure is observed. Of course, in vivo, and therefore in vitro, tumor cells are very sensitive to both cell intrinsic and external selective pressure. Therefore it is very important to monitor long term culture of tumor organoids because the population is dynamic and will evolve over time as will the in vivo tumor.
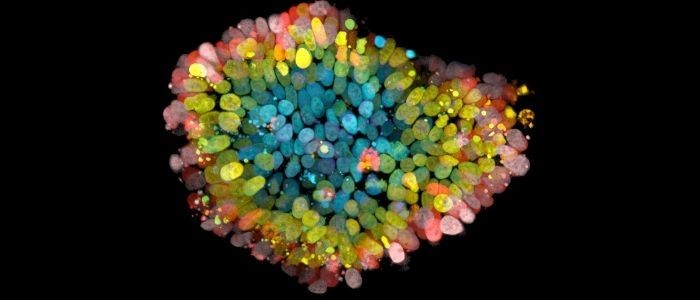
Which types of microscopes are used to observe 3D cell cultures?
Kalpana: 3D cultures can be observed using a range of microscopes and are dependent on what you are interested in observing and resolution. Inverted light microscopes, confocal and high content imagers are some examples.
Marta: We always use confocal microscopy for whole-mount immunofluorescence. Spinning disc confocal works well for time-lapse experiments of small organoids. Bigger organoids would require technologies that allow deeper penetration, for example light-sheet microscopy.
Has anyone conducted single-cell sequencing on patient-derived organoids and compared their similarities and differences in cell populations and microenvironment?
Rob: There are a number of studies that have performed single-cell sequencing on organoids. A recent one by the Clevers lab (Beumer et al. Cell 2020) shows the identification of different populations of enteroendocrine cells in the intestine. A European consortium of the Human Cell Atlas project is studying differences between cells of the intestine and brain. These studies will characterize the cell population and their response to the environment.
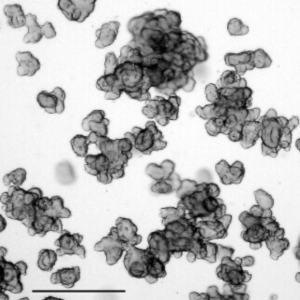
I did not hear anything about scaffold-free 3D cell culture. And will be happy to hear more experiences about it.
Kalpana: There are several techniques you can use to create 3D cultures without using scaffolds. Examples include using ultra low adhesion plates which have a round well bottom and ultra-low attachment coating, hanging drop plates as well as rotating bioreactors, micro-patterned plates and magnetic levitation.
Marta: Scaffold-free 3D cell culture is used for example to make embryoid bodies. This is a technology that allows you to generate aggregates of embryonic stem cells that can spontaneously differentiate and generate a collection of differentiated cells. Embryoid body formation just requires a non-adherent plate and the right media composition.
Which 3D cell culture method is more suitable for studying metastasis or invasion?
Kalpana: One method commonly adopted model is of single tumor spheroid invasion into an extracellular matrix such as Matrigel or Collagen. Here a single spheroid is created in a low adhesion plate, followed by direct addition of Matrigel into the same well, which provides a semi-solid matrix for the tumor cells to invade. The advantages of this method include precise control of the spheroid size allowing you to mimic the defined micro-regions of metastatic solid tumours and since the invasion assay is performed in situ there is no need to transfer the spheroid to a second plate which is common with other methodologies. This method is also highly compatible with automated live-cell analysis.