Icy veins: a new 3D printing method for building artificial blood vessels
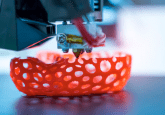
Researchers are using ice as a template for the 3D printing of artificial blood vessels in engineered tissues, which could one day be utilized for artificial organ transplants and drug testing.
A group of scientists has demonstrated the potential of 3D ice printing for creating blood-vessel-like structures. Feimo Yang, a graduate student in the labs of Philip LeDuc and Burak Ozdoganlar at Carnegie Mellon University (PA, USA), will be presenting this research at the 68th Biophysical Society Annual Meeting (February 10–14 2024; PA, USA).
Currently, more than 100,000 people in the United States are waiting for an organ transplant. Due to this demand far outweighing organ availability, there is a push for the development of lab-grown organs and tissues. However, one of the greatest challenges with tissue engineering artificial organs is the incorporation of functional blood vessel circuitry; previous artificial blood vessel designs haven’t mimicked the natural structure and function of biological vessels.
 Step aside 3D printing, there’s a new technique for biofabricating a heart
Step aside 3D printing, there’s a new technique for biofabricating a heart
The first biohybrid model of human ventricles has been used to answer a centuries-old question.
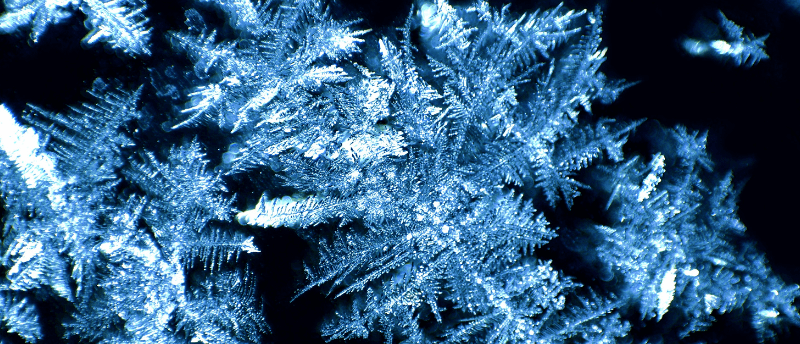
Recent research from Yang and colleagues has revealed the potential of 3D ice printing for developing artificial blood vessels that more closely mimic biological vessels. The team streams heavy water – water that’s hydrogen atoms have been replaced by deuterium, giving it a higher freezing point – onto a cold surface. In their system, the water never completely freezes on the printer, allowing scientists to create smooth 3D-printed structures.
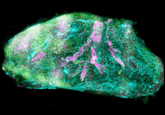
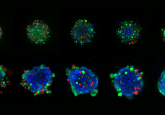
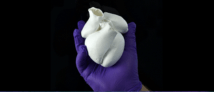
The 3D-printed ice templates are then used to mold the correct vessel-like shapes in a gelatin material termed GelMA, in which the templates are embedded. Exposing these molds to UV light causes the GelMA to harden and the ice to melt, leaving the researchers with networks of realistic blood vessels. Endothelial cells were added to the resulting artificial vessels and survived on the GelMA for up to 2 weeks.
In future, the team hopes to increase the time that cells can live on the gel. This could be a groundbreaking step for artificial organ transplantation and for testing the effects of drugs on blood vessels. Additionally, the team hopes that one day they will be able to place some patient cells on the gel vessels to see how they react to a drug treatment.