The top four misconceptions of personalized medicine

Laura Towart, Founder & CEO of My Personal Therapeutics LTD, discusses the four most common misconceptions in personalized medicine.
New technology is neither good nor evil, it’s just a matter of how people choose to use it. That’s why I’m using it to make sick people healthy again.
‘Personalized medicine’ refers to harnessing emergent technology and the latest medical know-how to segment patients into highly specific groups based on their similar traits. It’s not just about surface-level stats like age and gender, but it goes all the way down to people’s genetic makeup. What works well for one person in such a high-resolution segment becomes useful medical data for the others in the same segment. Personalized medicine lets healthcare providers tailor their prescriptions, treatments, or other interventions to the individual patient for maximum efficacy.
This medical methodology is already successfully turning the tide against conditions that were previously a death sentence and spawning a valuable new industry at the same time. But there are still those who challenge it. That’s why it’s time to tackle the top four misconceptions about precision medicine head-on.
The medicines we have work well enough. We don’t need anything new.
Try telling that to a patient whose chemotherapy treatment isn’t working, or to someone taking two, three, or more medications for their own medical condition. These approaches are like going fishing with a bomb. They represent a “one size fits all” mentality that we shouldn’t have to accept in 2019.
Learning to love personalized medicine for cancer, for example, requires the understanding that cancer is not a single disease. It’s actually 200 or 300 different diseases, so you can’t attack them all with just a single drug. A course of treatment that successfully counteracts one type of cancer might do nothing for another. That same treatment could even make a different type of cancer worse. That’s why we need to develop a specific treatment for every one of them, and this is exactly the approach that personalized medicine embraces.
BioTechniques Online Event: Advancing Precision Medicine 2019
If someone has a copy of my DNA, they can plant it at a crime scene and get me in trouble.
Personalized medicine relies on harvesting individual medical and genetic data in order to work. While collecting that data can lead to significant improvements in a patient’s health, it’s also a deep cause for privacy concerns (and maybe even some sci-fi flavored paranoia).
You only need to check out the Precision Medicine Initiative, an endeavor launched during the Obama administration that unites the National Institute of Health and a number of other research centers to identify best practices within personalized medicine. Yes, there are very valid concerns about how an individual’s data might be used beyond making the patient healthy, but the clear messaging from the powers that be is that this is strictly about improving health. It’s not about selling information to insurance companies, and it’s not about cloning people.
Congressional hearings on things like cryptocurrency and Facebook can be painful to watch. These events tend only to serve as a demonstration of how little the world’s lawmakers understand these topics. But the government has a good track record when it comes to medicine, perhaps because it understands that a healthy nation is a strong nation.
In the case of personalized medicine; that means the government also understands that this data requires its own kind of privacy.
It’s useless to learn that you have a gene mutation with no course of action attached to it.
It can be deeply unpleasant to learn that you have a mutation of the BRCA gene that’s linked to breast cancer, for example. But the argument that “not knowing” is better than “knowing” just isn’t compelling to a scientist.
In personalized medicine (or any other field of science), having more data helps us paint a fuller picture of the world — the quantity of knowledge is related to its quality. The more we know about someone’s specific health and existing medical idiosyncrasies, the better treatments we can provide for them.
Scientists aren’t exactly willing to hide from data. Everything matters until we know it doesn’t.
“Not only has precision medicine already made a significant difference in the lives of individual patients, but it’s given medical professionals a new set of tools for solving problems that would have previously stumped them.”
Personalized medicine depends on experimental models that aren’t similar enough to humans.
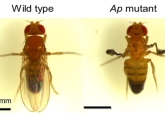
The classic image of a science experiment usually involves rats or mice, but these furry friends aren’t very compatible with personalized medicine methodology. It would require introducing a number of genetic mutations or cancer cells from human cancer patients into their system, then observing how different drugs work to counteract them. But this strategy is not suited for high-throughput drug screening. You can’t effectively work this method on a colony of 400,000 mice, which is why we use fruit flies — we can test each drug (or combination of drugs) in hundreds of flies as opposed to only three to five mice.
At the surface level, fruit flies are kitchen pests that have basically nothing to do with human biology, but they actually share up to 75% of the genes associated with human disease. They are, furthermore, the most genetically malleable organism out there, capable of handling 15 or more mutations in the same organ. No other animal can do this, so fruit flies are completely practical for personalized medicine purposes. We can recapitulate an exact copy of a human patient’s tumor inside of a fruit fly, then experiment on the fly to see what kind of treatment works.
These flies also give us a valuable analog to see how a human body will metabolize and distribute a drug. For instance, a tumor generated in the fly gut better resembles a human colorectal tumor than a cancer cell culture. A tumor inside the body interacts with the microenvironment as well as with other organs in a long-range communication process, which helps explain the wasting syndrome associated with cancer. These interactions affect drug performance, but they’re not present in cancer cell cultures, therefore the real effect of a drug can’t be realistically measured.
Fruit fly lifespans are also very short, so we can use thousands of them at a time to get meaningful results very quickly. Ross Cagan (Icahn School of Medicine at Mount Sinai; New York, USA) is the professor and researcher who invented my company’s technology, and he likens this use of the fruit fly to programming a computer. He’d say we can program this computer by giving it the genes we want it to have, then generate output by doing drug screenings against those genes.
I welcome skepticism and pushback against personalized medicine because it only makes the field more robust. Not only has personalized medicine already made a significant difference in the lives of individual patients, but it’s given medical professionals a new set of tools for solving problems that would have previously stumped them.
At the end of the day, this is about healing sick people. It’s just that we want to use the best possible tools to do so.
People already trust computers — is it such a far leap to ask them to trust fruit flies too?