Single-cell mass cytometry for identification of rare cancer cell subtypes: an interview with Wendy Fantl & Veronica Gonzalez
We spoke to Stanford University’s Wendy Fantl and Veronica Gonzalez about their novel use of mass cytometry (CyTOF) to identify never-before-seen cell subtypes in high-grade serous ovarian cancer (HGSOC). They discuss their discoveries, use of CyTOF and the potential applications of this method to other tumors [1].
Wendy Fantl is an assistant professor at the Division of Gynecologic Oncology at Stanford University (CA, USA). Wendy received her BA in Biochemistry from the University of York (UK) and PhD in Protein Biochemistry from Rockefeller University (NY, USA) before becoming a post-doc and adjunct assistant professor at the University of California, San Francisco (CA, USA). Wendy has 16 years of experience working in Biotechnology and Pharmaceutical industries. Wendy’s passion is in the mechanistic understanding of intracellular signaling pathways, DNA damage and the host immune system and their role in malignancies with an “eye on the prize” of a clinically translational endpoint. Her current interests are to apply multi-parametric single-cell technology platforms to identify disease-causing cell subpopulations in ovarian cancer and other malignancies.
3864
Veronica Gonzalez Muñoz is a senior research scientist in the Nolan Lab at Stanford University (CA, USA). Veronica received her MSc in Molecular Biology from Stockholm University (Sweden), PhD in Experimental Medicine from the Karolinska Institutet (Sweden) before becoming a postdoctoral fellow in virology/immunology at the National Institutes of Health (MD, USA). Veronica specializes in viral and tumour immunology and systems biology single-cell analysis.
3863
What are the implications of using CyTOF to identify rare cancer cell subtypes?
Previously HGSOC had been studied by analyzing homogenized tumors. In this study, we analyzed multiple parameters simultaneously in intact single cells rather than cellular homogenates. This multi-parameter approach provides the opportunity to identify rare and subtly different cell subsets that are lost in bulk homogenates.
These cell subsets may be rare but they could be important in maintaining tumor growth and spread. By studying their biological properties, further light may be shed on important questions such as how HGSOC tumors evolve, metastasize and/or become resistant to drugs.
In our study, single-cell analysis enabled us to identify targetable pathways as well as a minority cell type, previously unrecognized, that correlated with poor prognosis. Focusing drug therapies on reducing or eliminating such cells has the potential to significantly improve the outcome of this deadly disease.
Can you tell us about CyTOF and its uses in your research?
Mass cytometry (aka Cytometry by Time Of Flight, CyTOF) is a technology that can simultaneously reveal cell identity and behavior and is therefore well-suited to reveal detailed biological and mechanistic information about the diverse cell types within complex tumor samples.
CyTOF technology relies on its ability to distinguish between antibodies conjugated to purified stable metal isotopes, rather than fluorophores used in traditional flow cytometry. The metal isotopes chosen are rare or absent in biological systems and therefore background signals from cellular components are minimal. Cells are introduced into a mass cytometer, an instrument that can be thought of as a combination between a traditional flow cytometer and a time-of-flight mass spectrometer (TOF-MS). Protein expression levels are quantified from the TOF-MS readouts of the metal isotopes associated with each antibody. In contrast to fluorescence there is minimal overlap between isotope readouts and currently up to 50 parameters can be measured simultaneously for each single cell.
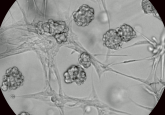
This capability for in-depth analysis of individual cells is what has made CyTOF such a powerful technology and it has been used to great effect for the study of cells in blood and the immune system. In our research we extended the use of CyTOF to examine single cells within HGSOC solid tumors. This necessitated the development of additional protocols to disaggregate freshly harvested tumor samples into viable single cells.
The multi-parametric attributes of mass cytometry allowed us to explore the notion that the well-established genetic and molecular complexity of HGSOC can be grouped into a more limited number of tumor cell types – each with potential weaknesses that can be targeted with specific cancer drugs.
What did you identify through analysis of intact cells using CyTOF that wouldn’t be possible with homogenized cell analysis?
One of our key findings in newly diagnosed HGSOC tumors was the identification of a pre-existing rare cell type that co-expressed vimentin, cMyc and HE4 and bore characteristics of metastatic cells. Higher numbers of these cells correlated strongly with early relapse. An assay enumerating these cells is now being developed to predict those patients likely to undergo early relapse. The clinical utility of such a test could help identify patients requiring immediate, more aggressive treatment options.
We also identified a second cell type expressing both E-cadherin and vimentin. This suggested the cells were on a pathway enabling their escape from the tumor compartment. When a malignant cell becomes metastatic and gains the ability to spread from its primary site to a secondary site, it stops expressing a cell-surface protein called E-cadherin and starts expressing vimentin. E-cadherin helps cells stick together through the formation of adherens junctions and in this way they are compartmentalized within their tissue of origin. Loss of E-cadherin with the subsequent gain of vimentin, an intermediate filament protein, allows a tumor cell “freedom of movement” enabling it to seed to a site that is distinct from the primary tumor. To-date such “transitional” cells had only been inferred to exist from analysis of tumor datasets or found in tumor animal models and cell lines.
Cell types that express both E-cadherin and vimentin, as identified in our HGSOC study, are strongly indicative of cells potentially “on the move”; this is doubtless a pathway for metastasis in other epithelial tumors. Their elimination could be the key to improving patient outcomes, since it is usually metastasis that makes cancer so deadly.
How difficult would it be to put this analysis into clinical practice?
The type of analysis we performed for HGSOC is in theory applicable to any malignancy. At present CyTOF is a research tool that has provided a new and important broad overview of HGSOC at the single-cell level by uniquely enabling the measurement of multiple proteins (>40) in one experiment comprising the analysis of up to 800,000 cells.
Computational analysis is an essential component of the technology and crucially distils the wealth of data into a few readily quantifiable key parameters, which when combined with patient outcome data, can be developed into clinically attainable tests using fluorescence-based flow cytometry or immunohistochemistry (clinically approved methodologies). Examples of potential tests are to identify patients susceptible to early relapse (as in our study) or response to a particular drug.
Can your discoveries from this study on HGSOC be applied to studies of other solid epithelial tumors?
Yes, this discovery-based approach to identify meaningful clinical correlates is transferrable to other solid tumors, especially now that there are an ever-increasing number of centers with access to CyTOF technology. Of course adjustments to the CyTOF antibody panel used to interrogate each of the different tissue malignancies will have to be made so as to match the recognized biology of the tumor types. However, our computational tools are directly transferable as are our pre-analytical guidelines for preparation of viable tumor single-cell suspensions.
One of the most illuminating pieces of data from our study is the ability to demonstrate “bad players” that pre-exist in newly diagnosed tumors (In our HGSOC study, cells co-expressing vimentin, cMyc and HE4). If indeed a pre-existing poor-prognosis cell phenotype is a general paradigm in newly diagnosed tumors there could be significant implications when they are identified. In support of this paradigm, in a recent CyTOF study of pediatric acute lymphoblastic leukemia samples, the presence of a rare subset of tumor cells was shown to predispose patients to relapse [2]. In general, enumerating pre-existing “bad” cells could provide a focus for developing more specific treatment strategies for their elimination as well as a more reliable prognosticator for relapse.
What are some of the limitations of CyTOF and what is the next step for your research?
CyTOF analysis is dependent on single-cell suspensions and thus loses spatial context. New multiplex imaging platforms extend the multi-parameter capabilities of CyTOF by using tissue slices enabling the associated spatial context between cells to be maintained. Three multi-parameter imaging platforms: imaging mass cytometry [3], multiplex ion beam imaging [4] and co-detection by indexing [5] provide critical information about the immune and stromal cell types surrounding these bad players and in so doing provide a potential opportunity to destroy both the tumor cells and their environment.