Exposing the circulatory impacts of COVID-19 with vascular organoids
Researchers have developed human-derived vascular organoids that can be infected with SARS-CoV-2 to investigate its impact on blood circulation, revealing a potential target for therapeutic development.
A recent research collaboration between Cincinnati Children’s Hospital Medical Center (OH, USA) and Tokyo Medical and Dental University (Japan), led by Takanori Takebe (of both organizations), has successfully developed vascular organoids to investigate the circulatory effects of COVID-19. Using these models, the team has been able to identify key mechanisms involved in the disruption to blood caused by SARS-CoV-2 and piece together a potential therapeutic solution.
When COVID-19 first ripped through the globe, one of the key factors identified in its deadly pathogenesis was the impact it had on the circulation of blood in acutely ill patients; both deep vein and microvascular thromboses were observed, alongside pulmonary embolisms. Unfortunately, the mechanisms behind these symptoms were not understood and traditional rodent model studies were of no help, as the rodent response to infection with SARS-CoV-2 was too disparate from our own.
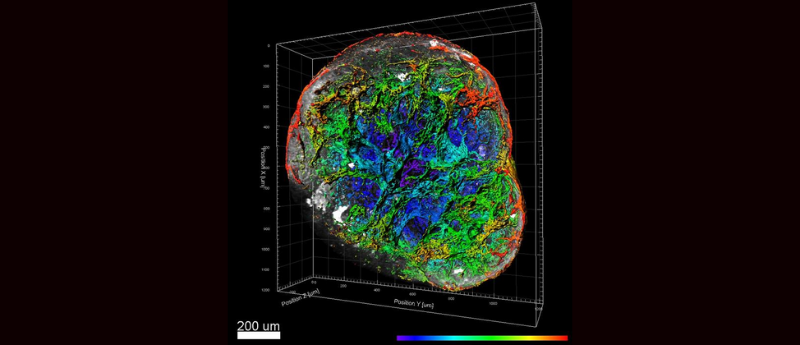
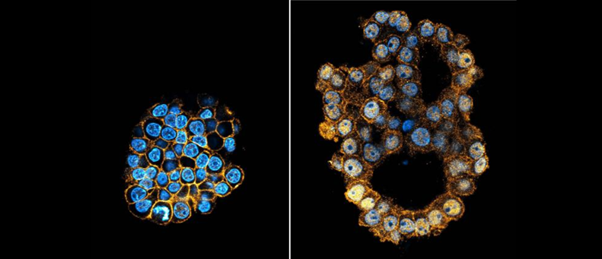
In order to address this gap in our understanding and to facilitate the development of more effective therapeutics for COVID-19, the research team set out to design a more appropriate model to investigate the mechanisms responsible for the circulatory effects of the disease. To do this, they successfully developed infection-competent human induced PSC (iPSC)-derived vascular organoids, dubbed iVOs.
 Base editing for more efficient and representative organoids
Base editing for more efficient and representative organoids
Using base editing, researchers have been able to establish tumor organoids with multiple mutations more efficiently.
The team then conducted a longitudinal proteome analysis of critically ill patients’ serum alongside an analysis of single-cell transcriptomics data derived from the bronchoalveolar lavage fluid of three healthy controls, three moderate and six severe COVID-19 patients.
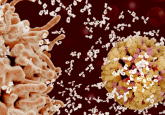
From this investigation the team found that a deviancy in the amplification cycle regulated by complement factor B and D (CFD) played a key role in COVID-19’s impact on the circulatory system. So, to combat the source of these symptoms, the team established a long-acting, pH-sensitive monoclonal antibody therapeutic that targets CFD. This monoclonal antibody was used to treat both the newly established vascular organoids and a cohort of macaque monkey models, both infected with COVID-19.
“After conducting many proteomic, genetic and other studies, we determined that the severe vascular damage and thrombosis associated with COVID-19 can be mitigated by a long-acting monoclonal antibody that targets the complement amplification cycle regulated by factor D (CFD),” Takebe revealed.
While these results were observed in both the organoid and macaque models, they were only mild. Next, the team want to investigate the development of a clinical-grade monoclonal antibody to target CFD with the hope that it will one day be used to successfully treat COVID-19.