Goodbye viral vectors, hello CRISPR
New technique successfully reprograms T cells without using viruses.
Researchers from the University of California, San Francisco (CA, USA) have genetically reprogrammed T cells using a CRISPR gene-editing technology. The method could accelerate both research and cell therapy development for a range of diseases.
The technique sees quantities of T cells, DNA and the CRISPR “scissors” mixed together and electroporated. The DNA is then precisely integrated at the cut site.
Traditionally, viruses have been used to transport DNA into cells, with some T cells engineered using viruses approved by the US FDA for cancer therapies. However, this process is difficult and expensive, and the gene insertion can be haphazard. These limitations cause a bottleneck in manufacturing, and the random gene insertion can lead to serious side effects.
This has lead researchers to explore new methods of reprogramming. However, previous attempts to introduce long stretches of DNA using electroporation and CRISPR into T cells have resulted in cell death.
“There has been 30 years of work trying to get new genes into T cells,” commented first author Theo Roth. “Now there should no longer be a need to have six or seven people in a lab working with viruses just to engineer T cells, and if we begin to see hundreds of labs engineering these cells instead of just a few, and working with increasingly more complex DNA sequences, we’ll be trying so many more possibilities that it will significantly speed up the development of future generations of cell therapy.”
The key to the success of the new techniques is the ratio of T cells, DNA and CRISPR, and the electrical field parameters. The ratios were discovered following a ‘Herculean’ effort of trial-and-error.
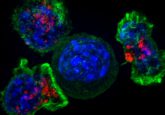
The team demonstrated their method shows low levels of off-target effects by labelling T cell proteins with GFP with high specificity. They then went on to repair an IL2RA defect in T cells from children with a severe autoimmune disease that was resistant to treatment.
Further experimentation saw normal human T cells given receptors designed to seek out melanoma cells. The cells specifically targeted melanoma in vitro. This translated into melanoma mouse models, with the cells moving to the mouse’s tumor and showing anti-cancer activity.
The new technique was able to create custom T cell lines in a little over a week, and has allowed the lab to take on more expensive or difficult experiments. “We’ll work on 20 ‘crazy’ ideas,” Roth said, “because we can create CRISPR templates very rapidly, and as soon as we have a template we can get it into T cells and grow them up quickly.”
“This is a rapid, flexible method that can be used to alter, enhance, and reprogram T cells so we can give them the specificity we want to destroy cancer, recognize infections, or tamp down the excessive immune response seen in autoimmune disease,” explained Alex Marson, senior author of the study. “Now we’re off to the races on all these fronts.”