Who are 2020’s scientific Nobel Prize winners?

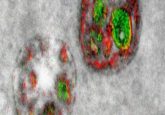
As the Nobel Prizes are announced this year, BioTechniques will cover the winners of the Physiology or Medicine, Chemistry and Physics prizes, their stories and the impact of their research. The 2020 Nobel Prize for Chemistry The Chemistry Nobel Prize will be written into the history books for a different reason this year as it became the first time two women have been jointly awarded the prestigious accolade. Emmanuelle Charpentier (Max Planck Unit for the Science of Pathogens, Berlin, Germany) and Jennifer Doudna (University of California, Berkeley, USA) have been recognized “for the development of a method for genome editing,”...
To view this content, please register now for access
Join our member community for FREE to access a collection of journal and online-only features, including:
- Exclusive access to educational videos, eBooks and insights into top BioTechniques journal articles
- The latest news and journal updates delivered straight to your inbox when you want it
- Personalized recommendations for the latest member-exclusive podcasts, interviews and expert opinions
- Priority registration to webinars, panel discussions and events
- Access to competitions and journal publication discounts, including 10% off open access fees when you sign up today!