More than meets the eye: how molecular aging can give an insight into health
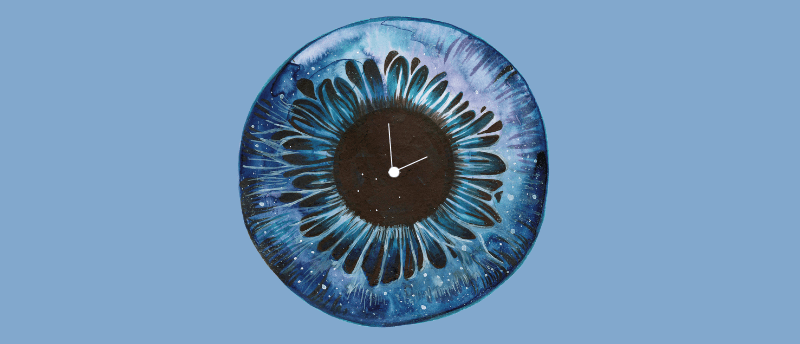
Eyes are not only the window to the soul but also to age and health status.
Researchers have developed a ‘proteomic clock’ capable of predicting a person’s age and disease status by analyzing the molecular age of their eyes. The Stanford University (CA, USA) team used liquid biopsies collected during routine eye surgeries to map nearly 6000 proteins from various eye cell types. From this dataset, an AI model estimated the age of healthy individuals and revealed that certain cell types show accelerated aging in individuals with eye diseases like diabetic retinopathy. Promisingly, proteins associated with Parkinson’s disease were also detected, offering a potential avenue for early Parkinson’s diagnoses.
Senior author Vinit Mahajan commented, “What’s amazing about the eye is we can look inside and see diseases happening in real time. Our primary focus was to connect those anatomical changes to what’s happening at the molecular level inside the eyes of our patients.”
Traditionally, studying the eye at the molecular level has proven challenging, in part due to the risk of irreversible damage to the eye when extracting tissue samples, as the eye is non-regenerative. Mahajan and his team therefore opted to use liquid biopsies taken from the aqueous or vitreous humor of patients undergoing eye surgery.
While non-invasive, liquid biopsies are limited in their capacity to measure large numbers of proteins within small volumes of fluid and are unable to trace the cellular origins of these proteins, a crucial aspect in disease diagnosis and treatment. To tackle this, the scientists integrated liquid biopsy proteomics with single-cell transcriptomics.
They identified proteins in liquid biopsies using aptamers – short, chemically modified DNA molecules that specifically bind to their protein targets. In total, 5953 proteins were identified, ten times the amount characterized in previous studies.
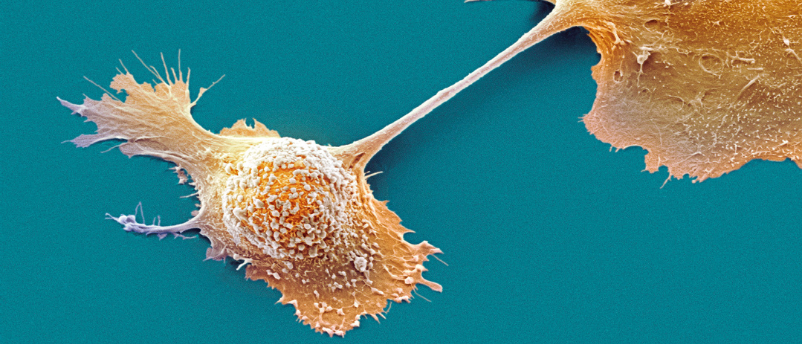
Novel 3D-printed tumor model enables better treatment outcomes
Complex heterogeneous tumors can be better understood with the aid of a new 3-dimensional modeling method.
They developed a software tool called TEMPO (Tracing Expression of Multiple Origins), which allowed them to trace the originating cell types of the identified proteins. Using TEMPO, they investigated the cell-type-specific expression of genes encoding for the proteins detected by integrating the proteomic data with published single-cell RNA sequencing (scRNA-seq) data of human ocular and extra-ocular tissues.
The team then built an AI model to predict the molecular age of an eye based on a liquid biopsy. While the model effectively estimated the age of healthy eyes, it showed substantial molecular aging linked to ocular diseases.
For instance, in individuals with diabetic retinopathy, disease progression correlated with the degree of molecular aging, with aging being accelerated by as much as 30 years for those with a severe (proliferative) presentation of the condition. On occasion, these signs of aging were present before individuals exhibited clinical symptoms and persisted in those that had been successfully treated.
The researchers also detected proteins associated with Parkinson’s disease that are usually identified postmortem. Existing diagnostic methods cannot test for these proteins, making Parkinson’s disease diagnoses particularly challenging. The discovery of these markers in eye fluid holds potential for earlier diagnosis and ongoing therapeutic monitoring.
These findings show that organs age at different rates, which could be organ- or even cell-specific. This insight could pave the way for advancements in clinical trial design and precision medicine. The authors even speculate that anti-aging drugs could be the future of preventative medicine.
Mahajan emphasized, “If we’re going to use molecular therapies, we should be characterizing the molecules in our patients. Reclassifying patients based on their molecular patterns and which cells are being affected could really improve clinical trials, drug selection, and drug outcomes.”
Going forward the team is going to expand their research by characterizing samples from a more extensive pool of patients and a wider spectrum of eye diseases. They also foresee the potential for their method to be extended to other challenging-to-sample tissues. For example, liquid biopsies of cerebrospinal fluid could provide insights into brain conditions, while synovial fluid and urine could offer valuable information on joint and kidney health.