Supporting life scientists during a pandemic: an interview with Candice Cox of Bio-Rad Laboratories
 Candice Cox is Global Marketing Manager of Immunoassays at Bio-Rad Laboratories (CA, USA). Cox has a BS in Biology from University of California, Los Angeles (UCLA; CA, USA) and started working in the life science industry about 20 years ago. She has had a varied career path, working in Pharma, R&D, project management and now marketing.
Candice Cox is Global Marketing Manager of Immunoassays at Bio-Rad Laboratories (CA, USA). Cox has a BS in Biology from University of California, Los Angeles (UCLA; CA, USA) and started working in the life science industry about 20 years ago. She has had a varied career path, working in Pharma, R&D, project management and now marketing.
How has Bio-Rad contributed to supporting life scientists during the COVID-19 pandemic?
On the life science side, we have developed research-use only SARS-CoV-2 immunoassays — the Bio-Plex Pro Human IgG SARS-CoV-2 Serology Assays — that measure IgG antibodies against four different SARS-CoV-2 proteins or protein subunits. These are nucleocapsid protein, and the receptor binding domain, spike 1 subunit and spike 2 subunit of the spike protein. This immunoassay can be run for research use only on a number of platforms: the Bio-Plex or Luminex 200, 3D or MAGPIX.
Bio-Rad also has RT-PCR assays, as well as droplet digital (dd) PCR assays for use under US Food and Drug Administration (FDA) Emergency Use Authorization (EUA) to detect the viral RNA and hence, an active SARS-CoV-2 infection.
Have you heard back from customers with any fascinating insights they have got from using these assays?
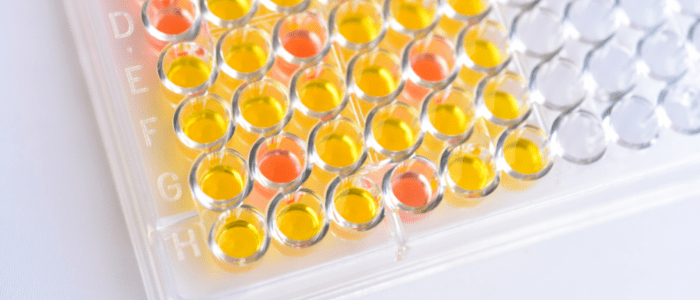
We only launched our serology assay for research use testing in February. So, it is pretty new to the market, but we did do a lot of early access testing and a lot of the positive feedback that we received was in terms of the ease of use with a single step dilution and ready-to-use controls, and fast time to results; they can get results from the assays in less than 3 hours.
In terms of their capability of measuring, antibodies were detected in research testing of samples from patients who were 7 days post-symptom onset all the way through to samples that were as far out as 3 to 6 months post symptom onset. Samples at later timepoints will continue to be collected and assayed in the study to understand the longevity of the antibody response. Researchers were able to measure the antibodies against all four of these proteins or protein subunits.
They were also matched at some points in the research studies to the levels of disease severity. So, if someone was hospitalized versus someone that was less ill with COVID-19, the trends that researchers expected to see were present. That was really positive for us to hear in terms of the potential utility and the sensitivity as well as the measurability of antibodies of varying levels over time.
How does Bio-Rad stand out in the SARS-CoV-2 immunoassays space?
Generally, offering solutions for research use only and diagnostic use has enabled us to address broader needs in the SARS-CoV-2 space.
On the diagnostic side there is an ELISA-based assay for use under EUA measuring antibodies against the SARS-CoV-2 nucleocapsid protein, which can be fully automated on an instrument called the EVOLIS. This ELISA is against total Ig, so it will measure antibodies with any of the isotypes: IgG, IgA or IgM.
For research use only, if you compare the Bio-Plex immunoassays to an ELISA, the advantage is the ability for researchers to measure multiple proteins in one well, in a shorter amount of time, and with a lower sample input volume needed.
The research use only Bio-Plex Pro SARS-CoV-2 Serology Assays from Bio-Rad are two to three times fastere than other companies that are developing similar assays on the same type of technology platform. In terms of utility, I think that there are some variations in the types of controls that are used. Our antibodies in our positive control for the IgG serology assays are specific to SARS-CoV-2, where others are not SARS-CoV-2 specific.
Tell me about Bio-Rad’s products that support vaccine development and population surveillance.
The Bio-Plex Pro SARS-CoV-2 Serology Assays can be used to measure exposure rates in a specific population, for research use. They can be used for population surveillance studies of anti-SARS-CoV-2 antibodies to understand local infection and exposure rates that may have been missed during active infection due to some mildly symptomatic or asymptomatic people not getting tested.
The Bio-Plex assays are useful as they allow you to measure more than just one protein, which becomes very relevant when you think about how vaccines are presenting the virus to our immune system. The first three vaccines to come out in the USA have been focused on presenting the spike protein to our immune system, and one of the ways researchers can distinguish whether or not someone has been either vaccinated or exposed naturally is looking at the types of antibodies that they have built up. The nucleocapsid proteins are not associated with these early vaccines but are presented during natural infection. For vaccines using more traditional inactivated virus, having four antigens can potentially allow researchers to capture a spectrum of antibody response versus measuring antibodies to only one antigen.
The assays can also be used in post market surveillance research studies for vaccines. Researchers want to be able to use an assay that is specific to SARS-CoV-2 and doesn’t cross react with any other virus. We have data collected in research studies showing that this assay is very specific to SARS-CoV-2 proteins and their subunits.
The other important aspect is that there are three isotype-specific 4-plex panels for detecting the different isotypes: IgG, IgA, IgM. Many of these population studies are designed not only to understand exposure rate but also to understand the profile and duration of the humoral response. This is similar for vaccine studies too — you want to understand how long an antibody response is measurable post-vaccination.
Since the start of the COVID-19 pandemic, how has Bio-Rad adjusted its approach and what has been adopted in that time period?
For the Life Science immunoassay business, we realized there were a few places we could pivot to provide support: in the basic understanding of the SARS-CoV-2 virus’s effect on the immune system, as well as in antibody prevalence studies and in the understanding of the immunogenicity of a vaccine.
For Bio-Rad, early on in Spring 2020, we launched the diagnostic ELISA-based Platelia SARS-CoV-2 Total Ab Assay for emergency use. We followed that up with assays and instruments for ddPCR and RT-PCR that were for research use and diagnostic testing. Then in early 2021, our research use only Bio-Plex Pro SARS-CoV-2 Serology Assays launched followed by an emergency use SARS-CoV-2 and Flu A/B RT-PCR test.
For our existing portfolio, we focused on highlighting the utility of these tools for SARS-CoV-2 research and therapeutic development. Vaccine research and development tools Bio-Rad also offers are multiplex immunoassays such as cytokine kits used in immune response profiling and raw beads and an amine coupling kit for developing custom assays, antibodies to develop assays for multiple technologies, flow cytometry for immunophenotyping, and electrophoresis and blotting to study host-cell-virus protein interactions.
Are there any new products coming out soon and what impact do you foresee these having on life science research?
Yes, we are soon going to launch the research use IgA and IgM serology assays for the Bio-Plex.
These assays will be really useful for those who are conducting basic science research, seroprevalence studies and even for vaccine research. It is important to understand the full spectrum of the humoral response, not just one specific type of antibody, such as IgG.
The assays can provide the bigger picture in terms of the humoral response, enabling the researcher to see from the beginning all the way through a study how long each of these antibody types persists. Originally, for seroprevalence studies, IgG was the antibody of key importance as it tends to be the one that is measurable for the longest time period.
However, researchers are now understanding the importance of monitoring additional antibodies to SARS-CoV-2, including IgA, which is involved in mucosal immunity and measurement of antibodies locally may lead to a better understanding of the impact of antibodies on disease severity. These findings can be used to develop therapeutics and other vaccine strategies in the future.
The opinions expressed in this Interview are those of the author and do not necessarily reflect the views of BioTechniques or Future Science Group.