Rare COVID-19 vaccine-related blood clot mechanism uncovered
Researchers identify a molecular interaction between the COVID-19 vaccine adenovirus vector and platelet factors which may be the cause of rare blood clots linked to the vaccine.
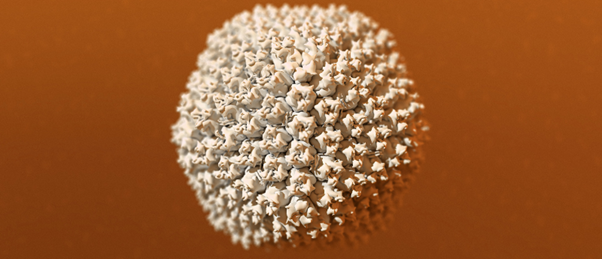
An international team of scientists from Cardiff University (UK) and Arizona State University (AZ, USA), alongside AstraZeneca (Cambridge, UK), have uncovered part of the mechanism involved in extremely rare blood clots linked to the administration of adenovirus COVID-19 vaccines. The research, led by first author Alexander Baker (both Arizona State and Cardiff University), used CryoEM technology to study the structure of the AstraZeneca vaccine adenovirus vector. The findings indicate that the adenovirus can bind to platelet factor 4 (PF4), involved in inflammation and wound repair, and may be the cause of the rare blood clots.
Vaccine-induced immune thrombotic thrombocytopenia (VITT), blood clotting, is a condition very rarely seen in a small number of people after administration of the Oxford-AstraZeneca or Johnson & Johnson vaccines. Scientists have speculated that the occurrence of the rare blood clots could be linked to the viral vector, used to elicit a protective immune response, as this unusual side-effect does not occur in people administered with the Moderna or Pfizer mRNA COVID-19 vaccines.
“VITT only happens in extremely rare cases because a chain of complex events needs to take place to trigger this ultra-rare side effect. Our data confirms PF4 can bind to adenoviruses, an important step in unraveling the mechanism underlying VITT,” co-author Alan Parker (Cardiff University) clarified.
 Whole-cell vaccines reimagined: a new method against recurrent UTI?
Whole-cell vaccines reimagined: a new method against recurrent UTI?
Recurrent UTIs may soon be a thing of the past as researchers develop encapsulating technology for whole-cell vaccines against Escherichia coli.
In order to examine the structure of ChAdOx1, the adenovirus vector in the AstraZeneca vaccine, the team utilized the flash-freezing technology CryoEM. The adenovirus samples were then bombarded with electrons to generate microscopic images of the viral capsid at the atomic level. The researchers found that the receptor of ChAdOx1 tightly binds with PF4 via electrostatic interactions. It is thought that this interaction between the adenovirus and PF4 and how it is interpreted by the immune system may cause the body to identify the complex as foreign, resulting in an immune response.
“With a better understanding of the mechanism by which PF4 and adenoviruses interact there is an opportunity to engineer the capsid, or outer shell of the vaccine, to prevent this interaction occurring. Modifying ChAdOx1 to reduce electronegativity may reduce the chance of causing thrombosis with thrombocytopenia syndrome,” Baker explained.
A spokesperson for AstraZeneca told the BBC that, “although the research is not definitive, it offers interesting insights and AstraZeneca is exploring ways to leverage these findings as part of our efforts to remove this extremely rare side effect.” They also stressed that blood clots were more likely to occur because of COVID-19 infection than as a result of the vaccine.
The team speculates that the VITT mechanism is a result of misplaced immunity as a downstream effect of the adenovirus binding with PF4 and aim to clarify whether this complex is inherently thrombogenic (prone to causing blood clots). Speaking to The Guardian (London, UK), Parker optimistically stated that, “we hope our findings can be used to better understand the rare side effects of these new vaccines and potentially to design new and improved vaccines to turn the tide on this global pandemic.”