Young bones, young blood, young brain
Transplanting bone marrow from young to old mice has been shown to maintain memory in the older mice by producing young blood cells, suggesting a new path for cognitive impairment treatment.
Transplanting bone marrow from young mice into their older compatriots has been shown to help the older mice maintain memory and learning functions longer than those given no transplant. The study, conducted at Cedars Sinai (CA, USA) and led by Helen Goodridge, adds to a growing understanding that aging blood cells contribute to neurodegeneration and highlights a possible new pathway for research into cognitive impairment treatment.
Existing studies have demonstrated that blood transfusions from young to old mice can protect against cognitive decline but the mechanism for this effect is not well understood. Goodridge and her team set out to explore this effect and establish more details regarding its mechanism.
In the first group, the researchers took 4-month-old mice and used them as donors for bone marrow transplants for 18-month-olds, a second group received transplants from mice their own age and a control group received no transplant at all. Six months later, the mice were subjected to laboratory tests of their special and working memory, activity level and learning ability. Mice who received a transplant from the four-month-old mice outperformed the control group and the group that received a transplant from other 18-month-old mice.
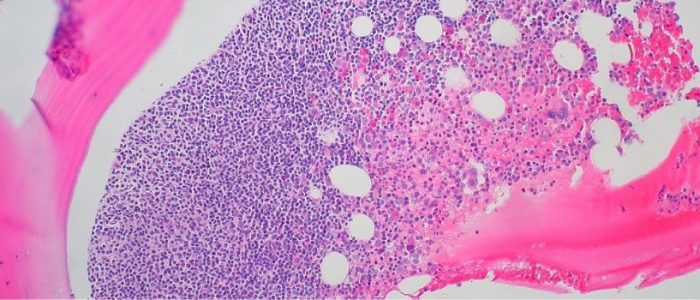
To dig deeper into this effect, the team then studied the hippocampus from each of the mice’s brains. They found that the density of synapses in the hippocampus of the mice that received the young bone marrow transplant was higher than the other two groups and that the microglia, a type of immune cell found in the brain, in the first group was more reminiscent of those found in younger mice, with smaller cell bodies and more protrusions than the microglia from the control and old transplant group.
“Our work indicates that cognitive decline in mice can be significantly reduced by simply providing young blood cells, which act on the brain to reduce the loss of synapses related to aging.”
On the completion of further tests, the research team found that this difference between the groups was due to the younger blood cells produced by the young bone marrow. These young blood cells reduced the activation of the microglia, which usually function to protect neurons but can become overstimulated and attack synapses, disconnecting them. This dampening of the microglia allowed more synapses to survive in the brains of the young transplant group, contributing to their enhanced brain performance compared to the other groups.
“We are entering an era in which there will be more elderly people in the population, along with an increased incidence of Alzheimer’s disease, putting a huge burden on the health system,” noted Clive Svendsen, co-senior author on the study. “Our work indicates that cognitive decline in mice can be significantly reduced by simply providing young blood cells, which act on the brain to reduce the loss of synapses related to aging.”
The study highlights that if this pathway can be confirmed in humans, the next challenge will be to convert these results into a treatment for humans, without using bone marrow transplants, which would not be feasible for treatment. Svendsen’s answer to this is to examine the possibility of “personalized” young blood stem cells as a potential cognitive impairment treatment that could be used to replace an individual’s aging blood stem cells, helping to stem the progression of cognitive decline.